Walter Keim
Almbergskleiva
64
NO-6657 Rindal, 19. February 2020
Norway
To
Professor Jari
Tiihonen
Karolinska Institutet
Department of Clinical
Neuroscience
S-171 77 Stockholm
Copy: Marc de Hert, Robert
Whitaker, Peter C. Gøtzsche, Professor, Michael Pascal
Hengartner, Sandra Steingard, Dr Joanna Moncrieff, Professor John
Read, <info@madinamerica.com>, Dr. Jeffrey Rubin
Corrigendum: 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study)
Sir,
I refer to the «11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study)» (1).
De Hert et al., 2010 «Do antipsychotic medications reduce or increase mortality in schizophrenia? A critical appraisal of the FIN-11 study.» (2) made the following comments:
«A number of methodological and conceptual issues make the interpretation of these findings problematic, including incomplete reporting of data, questionable selection of drug groups and comparisons, important unmeasured risk factors, inadequate control for potentially confounding variables, exclusion of deaths occurring during hospitalization leading to exclusion of 64% of deaths on current antipsychotics from the analysis, and survivorship bias due to strong and systematic differences in illness duration across the treatment groups»
Can you take into account these considerations and revise the FIN11 study?
Dr. Jeffrey Rubin discusses “Does “Antipsychotic” Treatment Reduce Risk of Death?” (3) considering many studies available and concludes: “The available research is not so perfect that we can make any definite conclusions regarding whether or not “antipsychotics” either increase or decrease mortality.” The group «no use of drugs» are not antipsychotic naive patients.
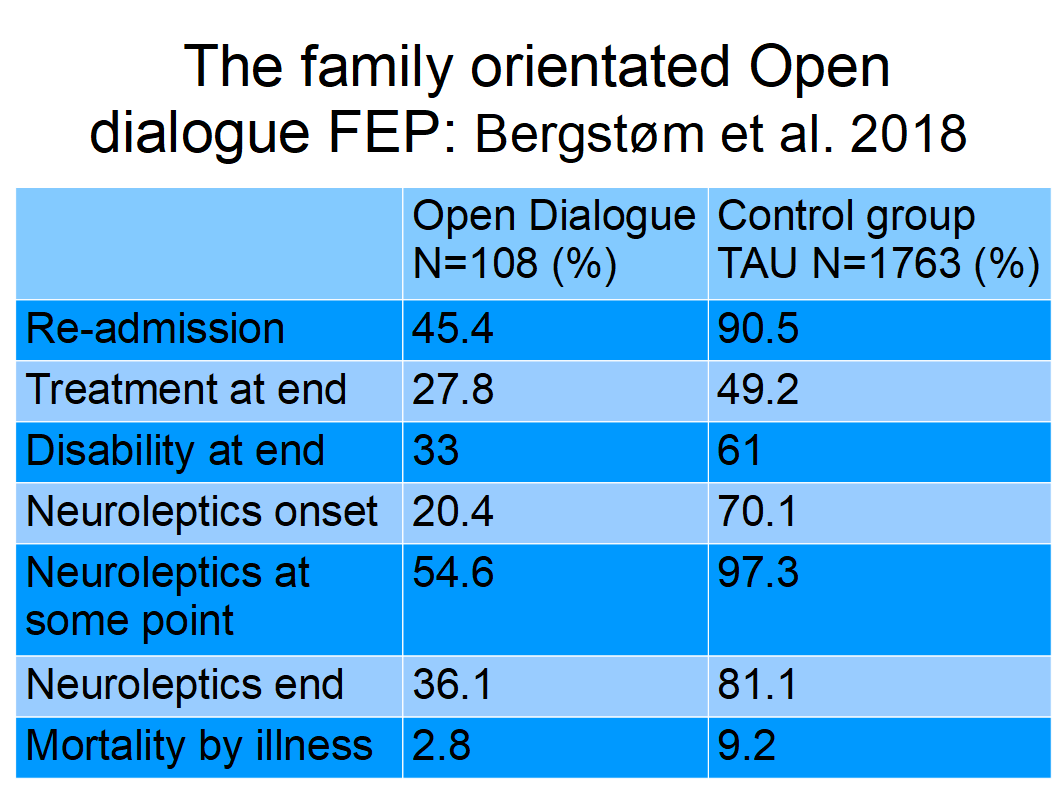
Bergstrøm et al. 2018 (4) found that 97,3% of “all Finnish FEP patients who had a follow-up of 19–20 years” received nevroleptics “at some point”. How come that approx. 25% person-years of FIN11 patients where on “no use of drugs”? Did “no use of these drugs” in outpatient care take drugs as inpatients in hospitals?
This letter may be a surprise, but I am trained as master of science in engineering i. e. physical engineering science and worked for the offshore industry applying quality assurance. So-called “deviation messages” and response to quality deviations are used to keep the records strait. Quality Assurance is also used in “quality of care” to “prevent, detect, or correct problems in quality”.
Looking forward to a corrigendum and revised study results.
Sincerely
Walter
Keim
https://sites.google.com/site/walterkeim/home
References:
Answer 20. February 2020, 11.42:
Emne: VS: Corrigendum 11-year follow-up of mortality in patients
with schizophrenia: a population-based cohort study (FIN11
study)
Dato: Thu, 20 Feb 2020 10:42:36 +0000
Fra: Jari Tiihonen
<jari.tiihonen@ki.se>
Til:
Walter Keim <walter.keim@gmail.com>
CC:
Marc de Hert, Robert Whitaker, Peter C. Gøtzsche, Professor,
Director, Institute for Scientific Freedom, Michael Pascal
Hengartner, Sandra Steingard, Dr Joanna Moncrieff, Professor John
Read, <info@madinamerica.com>, Dr. Jeffrey Rubin
Dear Walter,
Some of these
issues have been addressed more than 10 years ago (see
Authors' reply attached). If you read the 2009 paper you can see
that all deaths were included in the cumulative use analysis. These
issues have been studied thoroughly in a new study by Taipale
et al (attached).
Concerning Bergström et al. "At some parts" antipsychotic use includes also hospital use. Practically all patients with psychoses receive antipsychotics in hospital but it is not possible to obtain reliable detailed information on this from the national databases. Therefore, we studied current treatment only during outpatient care (which is more than 95% of all follow-up time). It is generally known that about 20% of patients do not use any antipsychotic after their first hospital treatment and do not get relapse. There are of course many patiens more who never use antipsychotic in outpatient care and get relapse and are hospitalized. Our results are based on official national statistics, and anyone having a reasonable study plan can apply for access to these data.
If you are interested in quality here is a tip for terminology: first episode psychosis is not the same as first episode schizophrenia, and concerning observational studies, one should not say that antipsychotics "incease" or "decrease" mortality. The right way to express this is that treatment is associated with higher/increased or lower/decreased mortality, since causality cannot be claimed for sure in observational studies.
Best regards,
Jari
---
Jari Tiihonen, MD, PhD
Professor
Department of Clinical Neuroscience
Karolinska Institutet
Stockholm, Sweden
E-mail: jari.tiihonen@ki.se
Attachment:
Tiihonen et al - 11-year follow-up of mortality - Authors reply - Lancet 2009
Taipale et al 2020: 20-Year Nationwide Follow-Up Study on Discontinuation of Antipsychotic Treatment in First-Episode Schizophrenia.
PS: May 2, 2020: Robert.Whitaker:
Do Antipsychotics Protect Against Early Death? A Review of the
Evidence. «In both psychiatric and non-psychiatric patients,
the use of antipsychotics doubles the risk of death in comparison to
patients who do not take the medications.»
The
“antipsychotics lengthen lives” research of Jari Tiihonen
is flawed in so many ways.
Minna Torniainen et al. 2015. Antipsychotic treatment and mortality in schizophrenia. “Among patients with schizophrenia, the cumulative antipsychotic exposure displays a U-shaped curve for overall mortality, revealing the highest risk of death among those patients with no antipsychotic use.”