Walter Keim
Almbergskleiva
64
NO-6657 Rindal, 6. August 2017
Rethinking
Antipsychotics(pdf) video Robert
Whitaker, February 2017
This question was asked as comment (second time here, third time here and forth time)
Thank you for answering the question about harm and benefit category.
“In the 1950s, when the drugs we now call ‘antipsychotics’ first came along, psychiatrists recognised that they were toxic substances that happened to have the ability to suppress thoughts and emotions without simply putting people to sleep in the way the old sedatives did” (Joanna Moncrieff, MD 13. August 2013; Deniker P. Compr Psychiatry 1960 Apr;1:92-102.). Mainstream psychiatry was uncomfortable with the notion that its principle treatment worked by being a neurological toxin and transformed it into a sophisticated, treatment.
Antipsychotic medications are now viewed as cornerstones for both the short-term and long-term treatment of schizophrenia. The evidence for symptom reduction will be critically reviewed. Are there benefits in terms of recovery?
Leucht et al. 2009 has found (How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials) the effect for short time treatment was 41% responded to drug compared with 24% to placebo NNT(Number Need to Treat)=6 (1). However this was looking at 50% or more reduction of symptoms on the Positive and Negative Syndrome Scale (PANSS).
Leucht et al 2012 looks at maintenance treatment with antipsychotic drugs. Between 7 to 12 month are covered. Hospitalisation was also reduced NNT=5. “This effect must be weighed against the side effects of antipsychotic drugs. Future studies should focus on outcomes of social participation and clarify the long-term morbidity and mortality associated with these drugs".
Bola et al. Cochrane.org 2011 (5) found just 5 studies with real placebo, i. e. RCT (Randomized controlled trial). One of them Rappaport et al 1978 found that umedicated patients managed better, e. g. readmission into hospital. NNH turned out to be 2.9 (NNH= number need to harm). The length of follow-up of this study was 3 years.
The Council of Evidence-based Psychiatry exists to communicate evidence of the potentially harmful effects of psychiatric drugs to the people (3).
Nancy Sohler et al. gives 2016 this summary: «For many years, this (…)clinicians’ belief in the need for long-term use of antipsychotic medications strong (Lehmann, 1966) that it has been impossible to design a sound observational study to address the question of efficacy or harm … (O)ur study also could not conclusively evaluate whether long-term antipsychotic medication treatment results in better outcomes on average. We believe the pervasive acceptance of this treatment modality has hindered rigorous scientific inquiry that is necessary to ensure evidence-based psychiatric care is being offered.»
So I understand there are nearly no RCT controlled studies (avoiding «cold turkey» problems) answering my question on recovery.
However is it possible to use other studies to evaluate effects based on other studies and real world results?
WHO Cross-Cultural Studies, 1970s/1980s found (Jablensky, A. 1992, Hopper, K. 2000): 16% of patients in the developing countries were regularly maintained on antipsychotics, versus 61% of the patients in rich countries. 63.7% of the patients in the poor countries were doing fairly well at the end of two years. In contrast, only 36.9% of the patients in the seven developed countries were doing fairly well at the end of two years. In the developing countries, 53% of schizophrenia patients were “never psychotic” anymore, and 73% were employed. In the rich countries, only 37 percent of the patients had good outcomes, and 59 percent had become chronically ill.
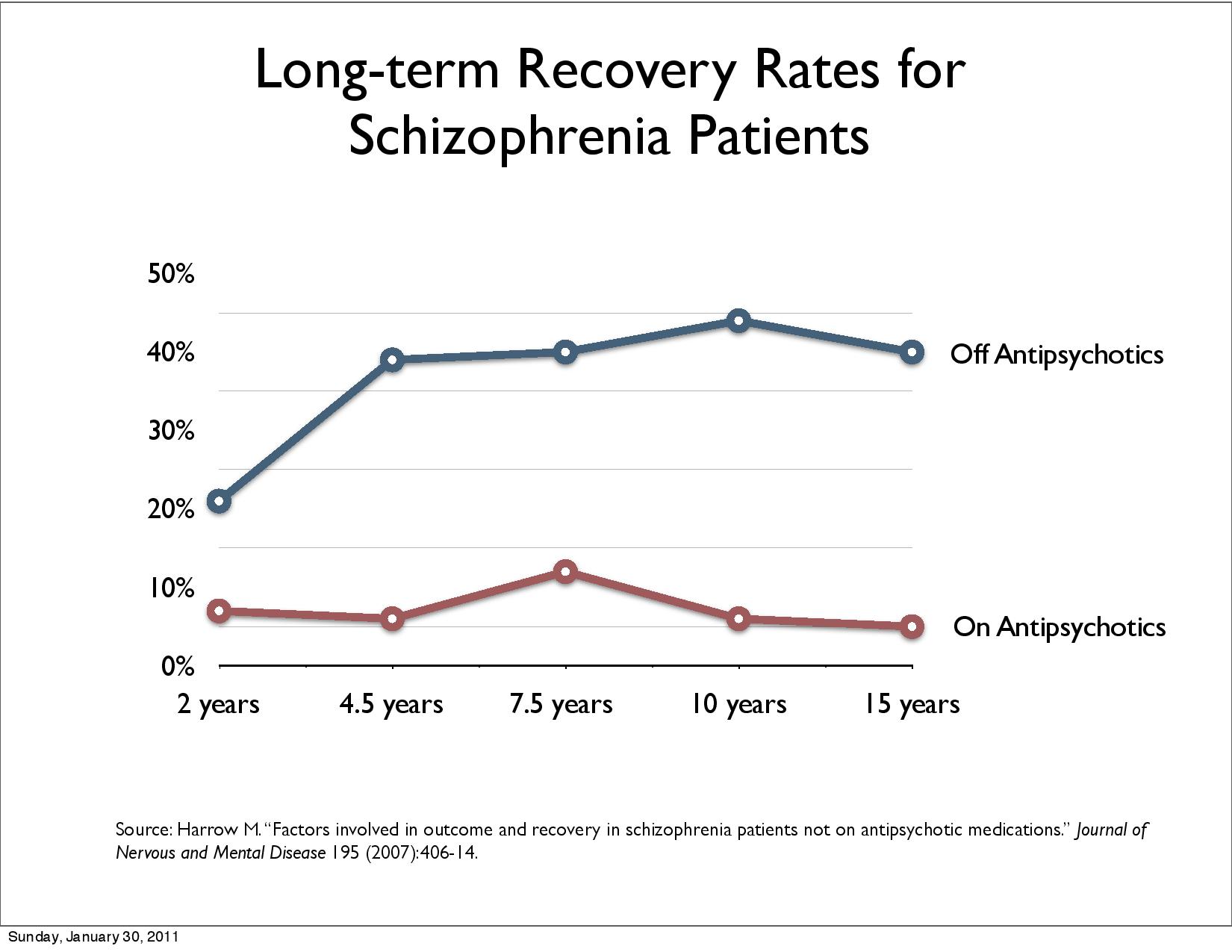
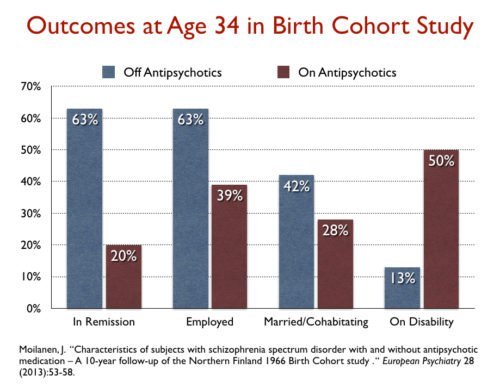
Naturalistic studies of e. g. Harrow, M. & Jobe, T.H. (2012), Harrow et al 2014 (11), Wunderink (4,7) and Wils et al 2017 show that patients do better without long-time antipsychotic medication. Harrow, M. & Jobe, T.H. (2017) concludes in “A 20-Year multi-followup longitudinal study assessing whether antipsychotic medications contribute to work functioning in schizophrenia”:
“Negative evidence on the long-term efficacy of antipsychotics have emerged from our own longitudinal studies and the longitudinal studies of Wunderink, of Moilanen, Jääskeläinena and colleagues using data from the Northern Finland Birth Cohort Study, by data from the Danish OPUS trials the study of Lincoln and Jung in Germany, and the studies of Bland in Canada,” (Bland R. C. and Orn H. (1978): 14-year outcome in early schizophrenia; Acta. Psychiatrica Scandinavica 58,327-338) the authors write. “These longitudinal studies have not shown positive effects for patients with schizophrenia prescribed antipsychotic for prolonged periods. In addition to the results indicating the rarity of periods of complete recovery for patients with schizophrenia prescribed antipsychotics for prolonged intervals, our research has indicated a significantly higher rate of periods of recovery for patients with schizophrenia who have gone off antipsychotics for prolonged intervals.”
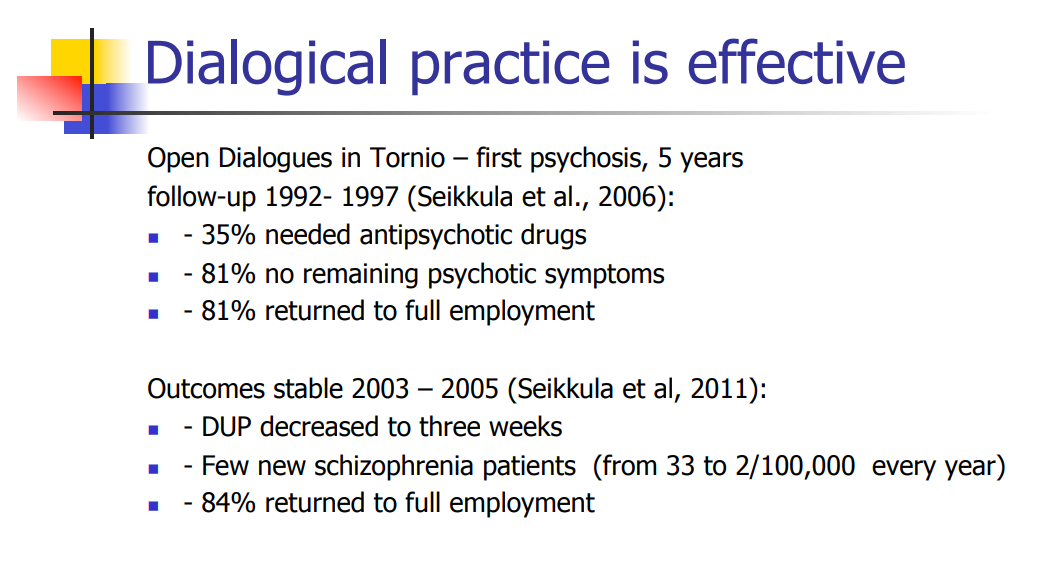
Jaakko Seikkula et al 2010 (Journal Psychosis Volume 3, 2011 - Issue 3) has reported on long-term outcome of first-episode psychotic patients treated with Open Dialogue Therapy in Western Lapland approx. 80% recovery (6). “Showing the benefit of using not much medication supported by psychosocial care.” 19% were on disability allowance or sick leave with 17% ongoing neuroleptics. Sveberg (2001) reported 62% on disability allowance or sick leave following standard care and 75% ongoing neuroleptics (11). Disability allowance or sick leave goes up more than 40%. Open dialogue reduced the incidents of psychosis from 33 to 2 per 100 000 annually.
The effect of cognitive therapy (8) and psychotherapy (9) is documented.
Bjornestad, Jone et al. 2017 reported “Antipsychotic treatment: experiences of fully recovered service users”: “(b)etween 8.1 and 20% of service users with FEP achieve clinical recovery (Jaaskelainen et al., 2013)” under the profession’s current protocols.
Approx. 60% or so of first-episode patients may recover without the use of antipsychotics (Whitaker 2017).
In order to maintain the narrative of antipsychotics being “effective” schizophrenia is falsely declared chronic i. e. drug dependence is preferred over recovery.
Now I know this guess is not exact science, but does it seem that approx. 40% of patients subject to regular medication (e. g. in Norway “National guideline for diagnosis, treatment and follow-up of individuals with psychotic disorders”) loose long-term recovery compared to non-medicated patients?
Would this be a fair guess of the long-term effect of antipsycotics on recovery?
John R Bola. 2005 (Medication-Free Research in Early Episode Schizophrenia: Evidence of Long-Term Harm?) found more then 4 studies showing positive effects of some weeks medication free treatment after some years.
There is research that shows evidence for drug-free alternatives.
Effects of physical activity for diagnoses schizophrenia is documented by Gorczynski P, Faulkner, G 2010. «Two trials compared exercise to standard care and both found exercise to significantly improve negative symptoms of mental state (Mental Health Inventory Depression:1RCT, n=10, MD 17.50 CI 6.70 to 28.30, PANSS negative: 1RCT, n=10, MD -8.50 CI -11.11 to -5.89).»
Both Rathod et al 2010, Sarin et al 2011 and Swati et al 2011 show evidence of cognitive therapy for schizophrenia. Hutton P, Taylor PJ 2014 "Cognitive behavioral therapy for psychosis prevention: a systematic review and meta-analysis" compares medicated and unedicated and finds that CBT is associated with a reduced risk of transition to psychosis.
Morrison et al. 2012 (9) concludes "A response rate analysis found that 35% and 50% of participants achieved at least a 50% reduction in PANSS (syptomer) total scores by than of therapy and follow-up respectively» this corresponds to NNT = 2 for « follow-up » with the aid of cognitive therapy, ie, only 2 patients must be treated for an additional patient to recover. With neuroleptics, it is 6 according to Leucht et al. 2009.
Morrison et al. 2014 shows in "Cognitive therapy for people with schizophrenia spectrum disorders not taking antipsychotic drugs: a single-blind randomized controlled trial." “INTERPRETATION: Cognitive therapy significantly reduced psychiatric symptoms and seems to be a safe and acceptable alternative for people with schizophrenia spectrum disorders who have chosen not to take antipsychotic drugs.”
Jauhar et al. 2014 «Cognitive-behavioral therapy for the symptoms of schizophrenia: systematic review and meta-analysis with examination of potential bias» shows therapeutic effect.
“Experiential Competence” writes April 28, 2014: "Psychotherapy for psychosis works" and refers to Michael Balter's "Talking Back to Madness" in the prestigious journal Science 14 Mar 2014: Vol. 343, Issue 6176, pp. 1190-1193. DOI: 10.1126 / science.343.6176.1190.
Spectrum Disorders Fønhus MS, Fretheim A, Johansen M. has in "Drug-free Measures in Mental Health Protection" (Note from 2016. Oslo: Public Health Institute, 2016) found many drug-free treatments.
Paul M. Grant et al., 2017, shows in the "Six-Month Follow-Up of Recovery-Oriented Cognitive Therapy (CT-R) for Low-Functioning Individuals With Schizophrenia" in a randomized study that "CT-R produced durable effects that were present even among individuals with the most chronic disease. "
This illustrates Klingberg's point (2012) that cognitive therapy has no evidence problem but an implementation problem.
Professor, Dr. Med. Peter C. Gøtzsche supports medicine-free treatment. Robert Whitaker looked 2016 at “Recovery Rates and Long-term Outcomes for Unmedicated Patients with Schizophrenia.” The findings where promising.
Patients have a right to know in advance to decide with informed consent the benefit of actual symptom reduction in the beginning at the price of long-term reduction of recovery. Where there is a risk there has to be a choice.
I would appreciate your answer based on your knowledge of studies. Thank you in advance.
Follow-up: Jim Gottstein: Schizophrenia Drugs Reduce Recovery Rates from 80% to 5% (Comparison Open dialogue/Harrow results)
Here is my answer to Ken: A shift of paradigm to Open dialogue achieves quadruple recovery rate, reduces schizophrenia per year to one tenth and disability allowance/sickness is reduced to one third.
References:
Leucht S,
Arbter D, Engel RR et al. How effective are second-generation
antipsychotic drugs?
A meta-analysis of placebo-controlled
trials. Mol Psychiatry 2009; 14:
429–447
https://www.nature.com/articles/4002136
Leucht S,
Tardy M, Komossa K, Heres S, Kissling W, Davis JM.2012 May
16;(5):CD008016. doi: 10.1002/14651858.CD008016.pub2.
Maintenance
treatment with antipsychotic drugs for
schizophrenia.
https://www.ncbi.nlm.nih.gov/pubmed/22592725
Council of
Evidence-based
Psychiatry
http://cepuk.org/unrecognised-facts/long-lasting-negative-effects/
Wunderink L,
Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in Remitted
First-Episode Psychosis at 7 Years of Follow-up of an Early Dose
Reduction/Discontinuation or Maintenance Treatment Strategy Long-term
Follow-up of a 2-Year Randomized Clinical Trial.
JAMA
Psychiatry. 2013;70(9):913-920.
doi:10.1001/jamapsychiatry.2013.19
http://jamanetwork.com/journals/jamapsychiatry/fullarticle/1707650
Bola JR, Kao D, Soydan H, Adams CE. Antipsychotic medication for early episode schizophrenia. 15 June 2011. http://www.cochrane.org/CD006374/SCHIZ_antipsychotic-medication-early-episode-schizophrenia
Robert
Whitaker. Harrow + Wunderink + Open Dialogue = An Evidence-based
Mandate for A New Standard of
Care:
http://www.madinamerica.com/2013/07/harrow-wunkerlink-open-dialogue-an-evidence-based-mandate-for-a-new-standard-of-care/
Dr. Lex Wunderink, MD, PHD of the University of Gronigen (Netherlands) speaks about his findings for long-terms use of antipsychotic drugs at the 2015 Yale Symposium: New Data and New Hopes Call for New Practices in Clinical Psychiatry. https://www.youtube.com/watch?v=RKeBjLG-ueY
Morrison AP,
Hutton P, Wardle M et al. Psychological Medicine. Volume 42, Issue 5
May 2012, pp. 1049-1056. Cognitive
therapy for people with a schizophrenia spectrum diagnosis not
taking antipsychotic medication:
an exploratory trial. Psychol Med 2012;
42: 1049 – 56
https://www.ncbi.nlm.nih.gov/pubmed/21914252?dopt=Abstract
Klingberg S,
Wittorf A. Evidencebased psychotherapy for schizophrenic
psychosis. Nervenarzt 2012; 83:
907-918.
https://www.ncbi.nlm.nih.gov/pubmed/22733380
Harrow M,
Jobe TH, Faull RN. Psychol Med. 2014 Oct;44(14):3007-16. doi:
10.1017/S0033291714000610. Epub 2014 Mar 24.
Does treatment of
schizophrenia with antipsychotic medications eliminate or reduce
psychosis? A 20-year multi-follow-up study.
https://www.ncbi.nlm.nih.gov/pubmed/25066792
Scientific Symposium. Pharmaceuticals – risks and alternatives. The 15th of October 2016 in Gothenburg, Sweden. Jaakko Seikkula, Professor of Psychotherapy, Clinical Psychologist, Finland. Naturalistic study designs for developing the system to reduced medication
Open letter
to the Directorate of Health, Knowledge Centre, Public Health,
Medicines Agency, Patient Safety Program, NORMENT, Experience
Expertise 12. February 2017:
Knowledge- and research-based
liquidation of current harmful psychiatric medication in favour of
evidence-based practice to promote recovery
http://wkeim.bplaced.net/files/open_letter_knowledge.html
Robert Whitaker: The case against antipsychotic drugs: A 50-year record of doing more harm than good. Medical Hypotheses Volume 62, Issue 1, 2004, Pages 5-1
Results of long-term use of antipsychotic drugs: