Paradigm Shift to Promote a Revolution of Treatment of Schizophrenia to Achieve Recovery. Walter Keim. Medical Research Archives https://esmed.org/MRA/mra/article/view/4866
To Sameer
Jauhar King's College London , Stephen M Lawrie Royal Edinburgh
Hospital
Copy: Donald C. Goff, M.D.,
Peter Falkai, M.D., Ph.D., W. Wolfgang Fleischhacker, M.D., Ragy
R. Girgis, M.D
I would like to comment Jauhar et al. 2023: What is the evidence for antipsychotic medication and alternative psychosocial interventions for people with acute, non-affective psychosis? "Antipsychotics are effective in treating acute psychosis and reducing relapse” on the background of how many are medicated and how long.
Summary: The evidence for antipsychotic medication is weak, and not sufficient for excessive medication of nearly all patients with diagnosis psychosis too long. Effects for acute treatment are small, uncertain and not relevant for recovery. Studies of relapse do not take into account possible abstinence and are not long enough to detect lack of effect.
Psychological interventions are underestimated. Open dialogue reached very good long-term treatment results using conscious reduced medication. United Nations Special Rapporteur on the right to health found excessive medication and World Health Organization (WHO) and United Nations High Commissioner for Human Rights (OHCHR) suggest how to solve these problems. The solution seems to be a shift of paradigm and revolution to obtain recovery (9). Jaakko Seikkula has already made the comment“In Defense of Open Dialogue Research”.
Table of Contents
Weak evidence for small effect of antipsychotics 1
Relapse protection time-dependent and disappears after 2 years 2
Conclusion for acute medication and maintenance 3
Open dialogue with less medication 4
UN Special Rapporteur on the right to health, WHO and UN OHCHR 5
Nearly all randomized controlled trials (RCT) use a “wash-out” period before randomizing to placebo or drug because it was wrongly considered unethical not to give antipsychotics. Both Carpender et al. 1977 and Bola 2011 found that studies with antipsychotics-naive participants are safe and therefore not unethical.
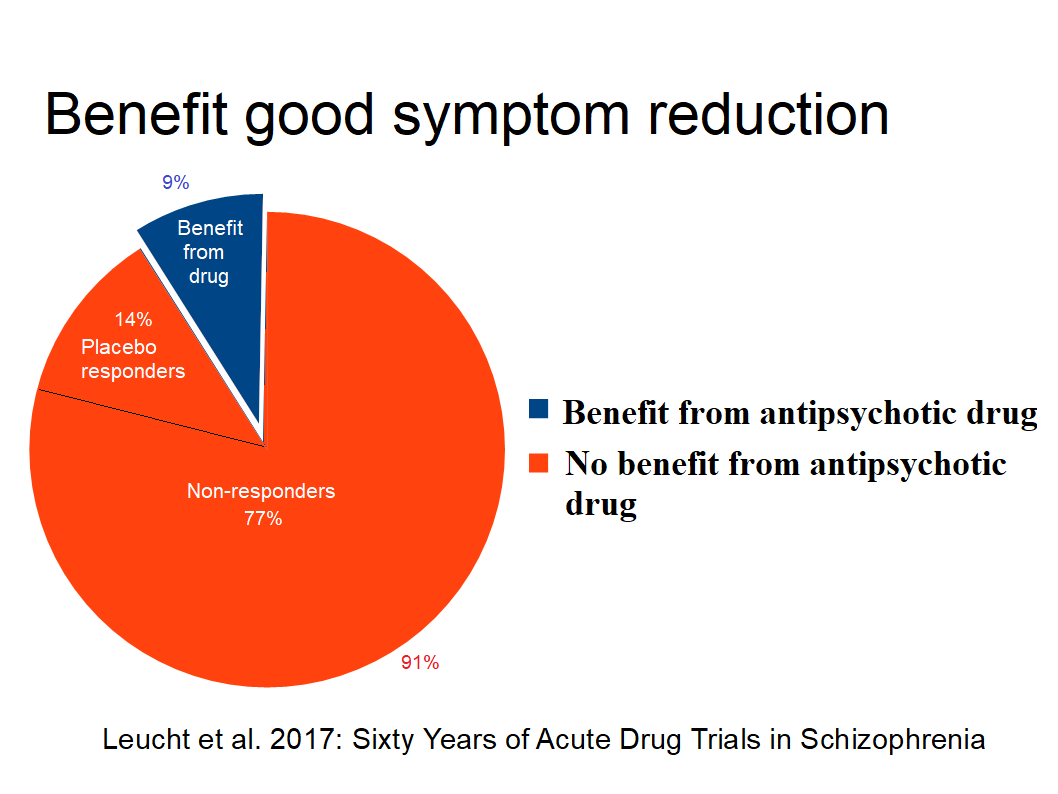
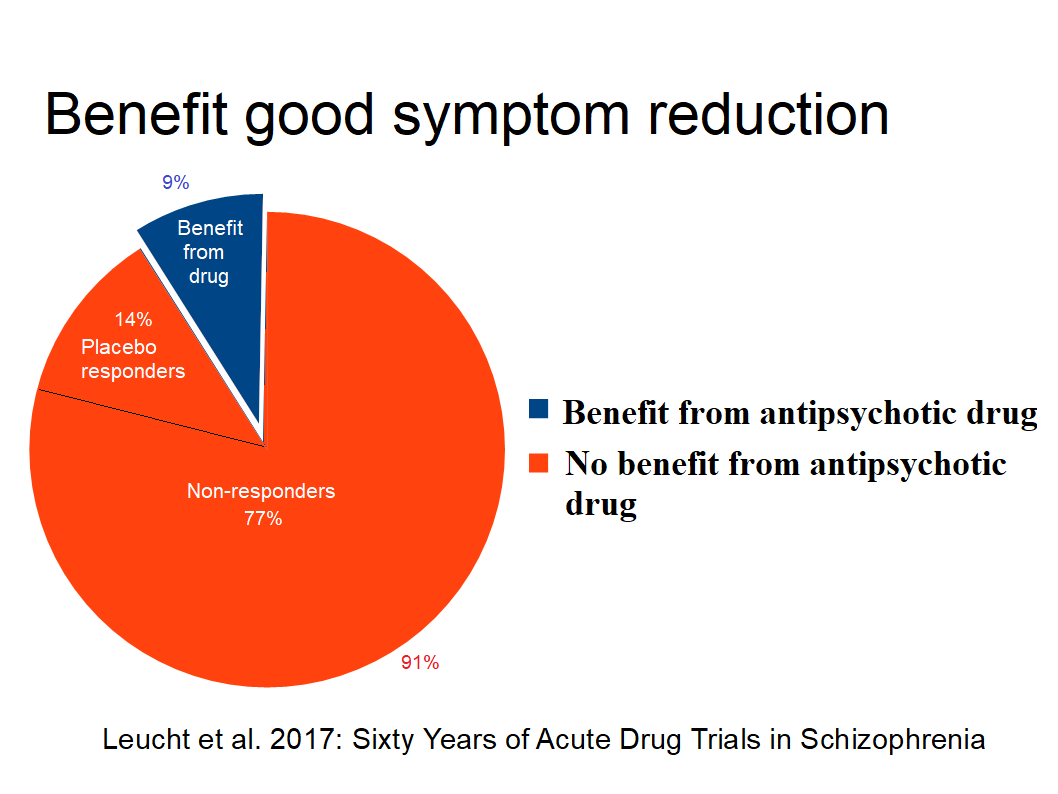
Leucht et al. found in 2017 summarizing 60 years of drug trials in acute schizophrenia 23% experiencing good symptom reduction, placebo response 14%, and 9% benefit i. e. 91% had no such benefit of drugs.
Dalsbø et al. (Norwegian Institute of Public Health) (1) concluded 2019: “ It is uncertain if antipsychotics compared to placebo affects symptoms in persons with early psychosis” because antipsychotic-naive participants are missing.
Iversen et al.(2) found 2018 in “Side effect burden of antipsychotic drugs in real life - Impact of gender and polypharmacy”: Use of antipsychotics showed significant associations to neurologic and sexual symptoms, sedation, and weight gain, and >75% of antipsychotics-users reported side effects.
Lindstrøm et al. (3) reports 2001 total of 94% of side effects for patients under maintenance treatment.
«The most striking result of the Clinical Antipsychotic Trial of Intervention Effectiveness (CATIE) study, which enrolled almost 1,500 individuals with chronic schizophrenia, was the high rate of treatment discontinuation (up to 74%) over the 18-month period of the trial and the short median time to discontinuation of treatment (about 6 months) in all phases of the trial.». The initial CATIE report 2005 has been cited in the literature over 1,600 times (Lieberman et al. 2011).
Danborg et al.(4) conclude 2019 that: “The use of antipsychotics cannot be justified based on the evidence we currently have. Withdrawal effects in the placebo groups make existing placebo-controlled trials unreliable.”
The strict claim of antipsychotic-naive research leaves the medication of nearly all patients with the diagnosis of schizophrenia without proper justification and, therefore, maintenance results without relevance because of possible withdrawal/abstinence effects.
According to Leucht et al. 2012 “nothing is known about the long-term effects of antipsychotic drugs compared to placebo. Future studies should focus on the,outcomes of social participation and clarify the long-term morbidity and mortality associated with these drugs.” The study was based on 7 to 12 month.
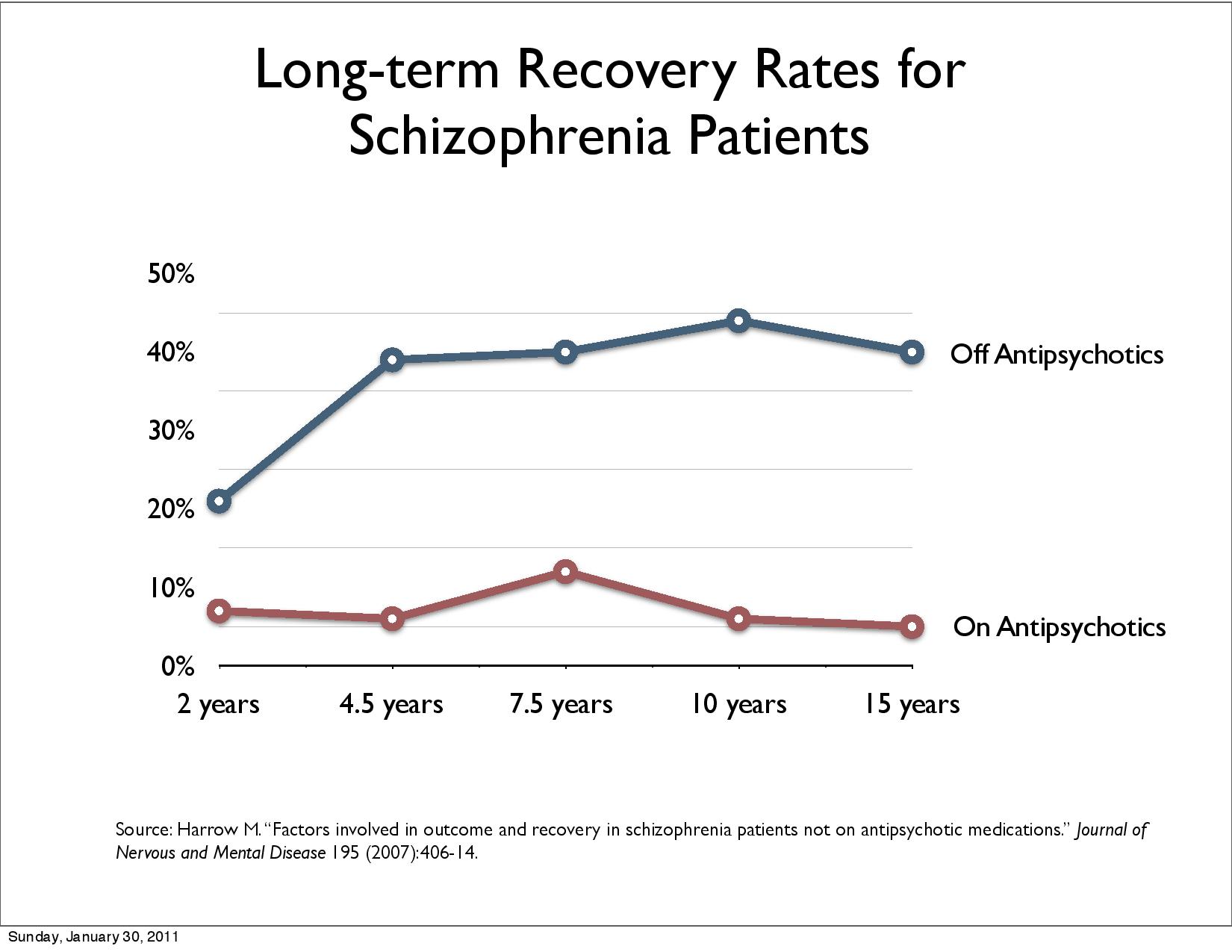
Schlier et al. 2023 (5) conducted the first meta-analysis pooling the long-term effects of antipsychotic maintenance versus discontinuation on functional recovery in people with schizophrenia spectrum disorders. The result was that the benefit of maintenance disappears after two years. The clinical experience that the disease returns on discontinuation is an illusion as abstinence is ignored.
Sohler et al. 2015 (6) found in “Weighing the Evidence for Harm from Long-term Treatment with Antipsychotic Medications, A Systematic Review” no evidence for long term treatment: “We believe the pervasive acceptance of this treatment modality has hindered rigorous scientific inquiry that is necessary to ensure evidence-based psychiatric care is being offered.”
This evidence for justifying medicating nearly all is already very weak, but there is no evidence at all for long-term medication.
9% of patients have a good acute symptom reduction benefit of antipsychotics. Adding placebo effect leaves 77% non-responders (Leucht et al. 2017). Maintenance studies mentioned fall short of taking into account possible abstinence effect and cover too short time. After 2 to 3 years no protective effect is observed. Apparently this evidence does not legitimate to choose antipsychotics as treatment for nearly all diagnosed psychosis. 94% of patients experience side-effects (3) lead to 74% stopped taking antipsychotics (Lieberman et al. 2011). Clinicians are uninformed and call this therefore nonadherence.
Open dialogue uses less medication and psychosocial interventions show better results. UN Special Rapporteur on the right to health criticizes excessive medication, WHO and UN OHCHR follow up with suggestions to solve the problem.
Bergström et al. 2018 compared Open dialogue patients in northern Finland with all FEP patients in Finland over a period of 19 years. Open dialogue (OD) uses neuroleptics for 20% of patients in the beginning, standard treatment (CG control group) 70%. 97,3 % of the CG get neuroleptics at some point. At the end, 36% of OD patients use neuroleptics, for CG it is 81%. Disability allowance, readmission and patients under treatment halves with OD. Randomization should guarantee that patients are evenly distributed among groups. This study is based on a “natural randomization” and the study discusses that the open dialogue area is comparable the rest of Finland with small discrepancies. Comparison with traditional RTC studies shows advantages of this study:
• No selection bias because all patients in both groups are included
• At onset only 20.4% of patients are medicated in the Open dialogue area i.e. 80% are antipsychotics naïve and avoids this weakness of traditional RCTs
• Disability, readmission, and patients under treatment reflects recovery better than symptom reduction
• long-term recovery is covered an area traditional RCTs do not cove
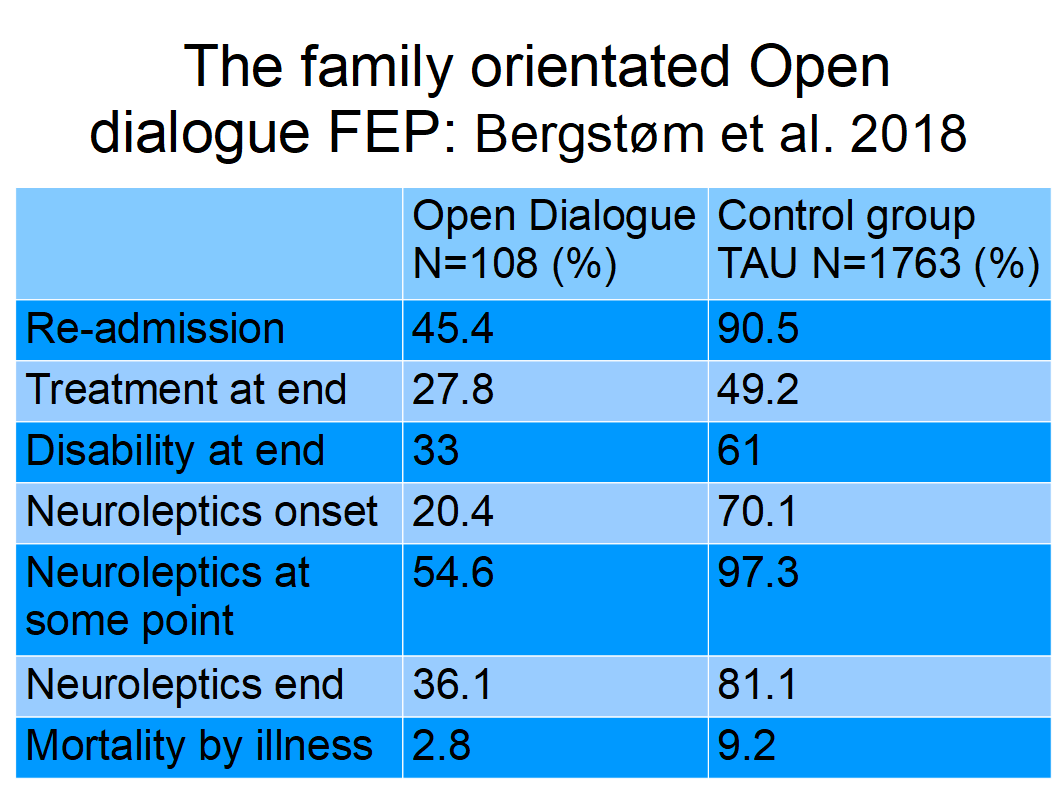
This is better evidence with higher effect than for antipsychotics without any evidence for log-term medication.
Medicine-free treatment, e.g. Basal exposure therapy BET (Number Needed to Treat NNT 1.9), Dialogue Therapy (Haram et al. 2018) (6) (NNT < 1.5) for GAF and Open Dialogue with more than half drug-free, i.e. psycho-social treatment have better effects than antipsykotics (AP) with NNT 11 for good acute symptom reduction.
United Nations Special Rapporteur on the right to health Mr. Puras has called for «World needs "revolution" in mental health care» due to "unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist" (7).
WHO (60) followed up with the “(n)ew WHO guidance (which) seeks to put an end to human rights violations in mental health care”: "This comprehensive new guidance provides a strong argument for a much faster transition from mental health services that use coercion and focus almost exclusively on the use of medication to manage symptoms of mental health conditions, to a more holistic approach that takes into account the specific circumstances and wishes of the individual and offers a variety of approaches for treatment and support". Compulsory Community Treatment Orders and forced injections of antipsychotics are ineffective and unethical. WHO mentions Basal exposure therapy (BET) as example for good practice.
The WHO-OHCHR guidance launched October 2023 seeks to improve laws addressing human rights abuses in mental health care (WHO-OHCHR 2023 (8) ) to support countries in reforming legislation in order to end human rights abuses and increase access to quality mental health care.
Treatment-As-Usual (TAU) did not improve patients recovery, mainly due to resistance to giving up excessive medication. Legislators can solve this deadlock by following OHCHR suggestions and removing legal permission for forced drugging. This could promote a shift of paradigm of treatment of schizophrenia towards recovery (9).
Rindal, 17. March
2024
Walter Keim
Netizen:
http://walter.keim.googlepages.com
KEIM,
Walter. Paradigm Shift to Promote a Revolution of Treatment of
Schizophrenia to Achieve Recovery. Medical Research Archives
https://esmed.org/MRA/mra/article/view/4866
References:
1. Dalsbø TK, Dahm, KT, Øvernes, LA, Lauritzen M, Skjelbakken T. [Effectiveness of treatment for psychosis: evidence base for a shared decision-making tool] Rapport 2019. Oslo: Folkehelseinstituttet, [Norwegian Institute of Public Health] 2019.
2. Iversen TSJ, Steen NE, Dieset I, et al. Side effect burden of antipsychotic drugs in real life - Impact of gender and polypharmacy. Prog Neuropsychopharmacol Biol Psychiatry. 2018;82:263-271. doi:10.1016/j.pnpbp.2017.11.004 Nov 7. PMID: 29122637.
3. Lindström E, Lewander T, Malm U, Malt UF, Lublin H, Ahlfors UG. Patient-rated versus clinician-rated side effects of drug treatment in schizophrenia. Clinical validation of a self-rating version of the UKU Side Effect Rating Scale (UKU-SERS-Pat). Nord J Psychiatry. 2001;55 Suppl 44:5-69. doi:10.1080/080394801317084428
4. Danborg PB, Gøtzsche PC. Benefits and harms of antipsychotic drugs in drug-naïve patients with psychosis: A systematic review. Int J Risk Saf Med. 2019;30(4):193-201. doi:10.3233/JRS-195063
5. Schlier B., et al. 2023. Time-dependent effect of antipsychotic discontinuation and dose reduction on social functioning and subjective quality of life–a multilevel meta-analysis. EeClinicMedicine Volume 65, 102291, November 2023. DOI:https://doi.org/10.1016/j.eclinm.2023.102291
6.. Sohler N, Adams BG, Barnes DM, Cohen GH, Prins SJ, Schwartz S. Weighing the evidence for harm from long-term treatment with antipsychotic medications: A systematic review. Am J Orthopsychiatry. 2016;86(5):477-485.doi:10.1037/ort0000106
7. The United Nations Special Rapporteur on the right to health, Dainius Puras “World needs “revolution” in mental health care – UN rights expert” online publication 06 June 2017. https://www.ohchr.org/en/press-releases/2017/06/world-needs-revolution-mental-health-care-un-rights-expert?LangID=E
8. WHO “New WHO guidance seeks to put an end to human rights violations in mental health care” online publication 10 June 2021. https://www.who.int/news/item/10-06-2021-new-who-guidance-seeks-to-put-an-end-to-human-rights-violations-in-mental-health-care
9. Keim, Walter. Paradigm Shift to Promote a Revolution of Treatment of Schizophrenia to Achieve Recovery. Medical Research Archives, [S.l.], v. 11, n. 12, dec. 2023. ISSN 2375-1924. Available at: https://doi.org/10.18103/mra.v11i12.4866