Paradigm Shift to Promote a Revolution of Treatment of Schizophrenia to Achieve Recovery. Keim, Walter. Medical Research Archives https://doi.org/10.18103/mra.v11i12.4866
To Donald C. Goff, M.D., Peter Falkai, M.D., Ph.D., W. Wolfgang Fleischhacker, M.D., Ragy R. Girgis, M.D Copy: Elisabeth C. Klæbo Reitan, Valentina C. Iversen, Henriette Riley, Anne Høye, Norwegian Psychiatric Association, Solveig Klæbo Reitan, Lars Lien formann i Norsk psykiatrisk forening
In «The Long-Term Effects of Antipsychotic Medication on Clinical Course in Schizophrenia» acute treatment and prevention of relapse is discussed.
Summary:
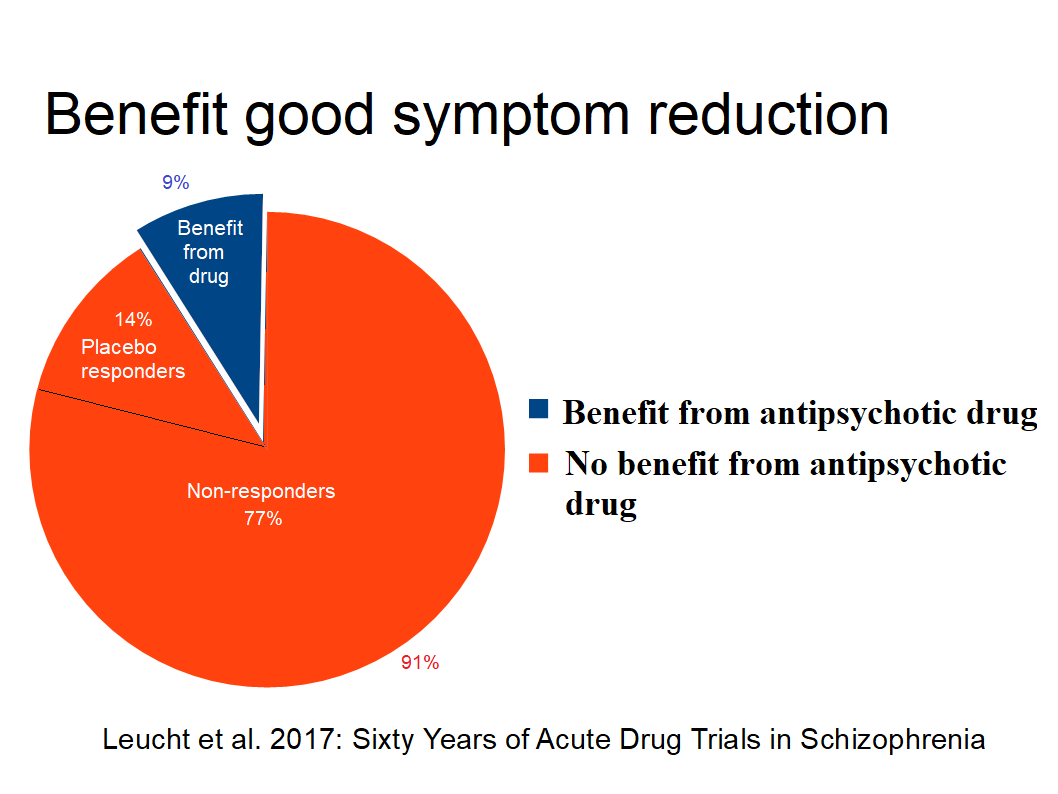
9% of patients treated with antipsychotics benefit with acute good symptom-reduction. However this effect is uncertain due to the lack of medication-naive i.e. wash-out period of placebo group. The aim of treatment according to laws is recovery and symptom-reduction is not necessarily contributing.
Maintenance studies are unreliable, i.e. the contribution of abstinence effect is not known. Most studies are too short and do not take into account that positive effects seem to last no longer than 2 to 3 years.
The evidence for antipsychotic medication is weak, and not sufficient for excessive medication of nearly all patients with diagnosis psychosis. There is no evidence for for long term treatment (Sohler et al. 2015).
Due to low effect and many side effects, many patients stop taking antipsychotics, seen as non-adherence by psychiatrists caused by a lack of insight. Many patients want medication-free treatment (Standal 20211) opposed by psychiatrists.
Treatment-As-Usual (TAU) did not improve patients recovery, mainly due to resistance to giving up excessive medication. Legislators can solve this deadlock by following OHCHR suggestions and removing legal permission for forced drugging. This could promote a shift of paradigm of treatment of schizophrenia towards recovery
Table of Contents
No strict evidence for initial treatment
Good acute symptom reduction for few patients
Maintenace treatment : Relapse protection time-dependent and disappears after 2 to 3 years
Open dialogue results encouraging
Patients reaction
Medication-free treatment 7
Human rights perspective leads to reasonable medicating
The summary for initial treatment says:
“The efficacy of antipsychotics for the initial treatment of psychosis is well established.”
However, nearly all randomized controlled trials (RCT) use a “wash-out” period before randomizing to placebo or drug because it was considered unethical not to give antipsychotics. Both Carpender and Bola 2011 found that studies with antipsychotics-naive participants are safe and therefore not unethical.
Dalsbø et al. (Norwegian Institute of Public Health)2 concluded 2019: “ It is uncertain if antipsychotics compared to placebo affects symptoms in persons with early psychosis” because antipsychotic-naive participants are missing.
Iversen et al.3 found 2018 in “Side effect burden of antipsychotic drugs in real life - Impact of gender and polypharmacy”: Use of antipsychotics showed significant associations to neurologic and sexual symptoms, sedation, and weight gain, and >75% of antipsychotics-users reported side effects.
Lindstrøm et al.4 reports 2001 total of 94% of side effects for patients under maintenance treatment.
Danborg et al.5 conclude that: “The use of antipsychotics cannot be justified based on the evidence we currently have. Withdrawal effects in the placebo groups make existing placebo-controlled trials unreliable.”
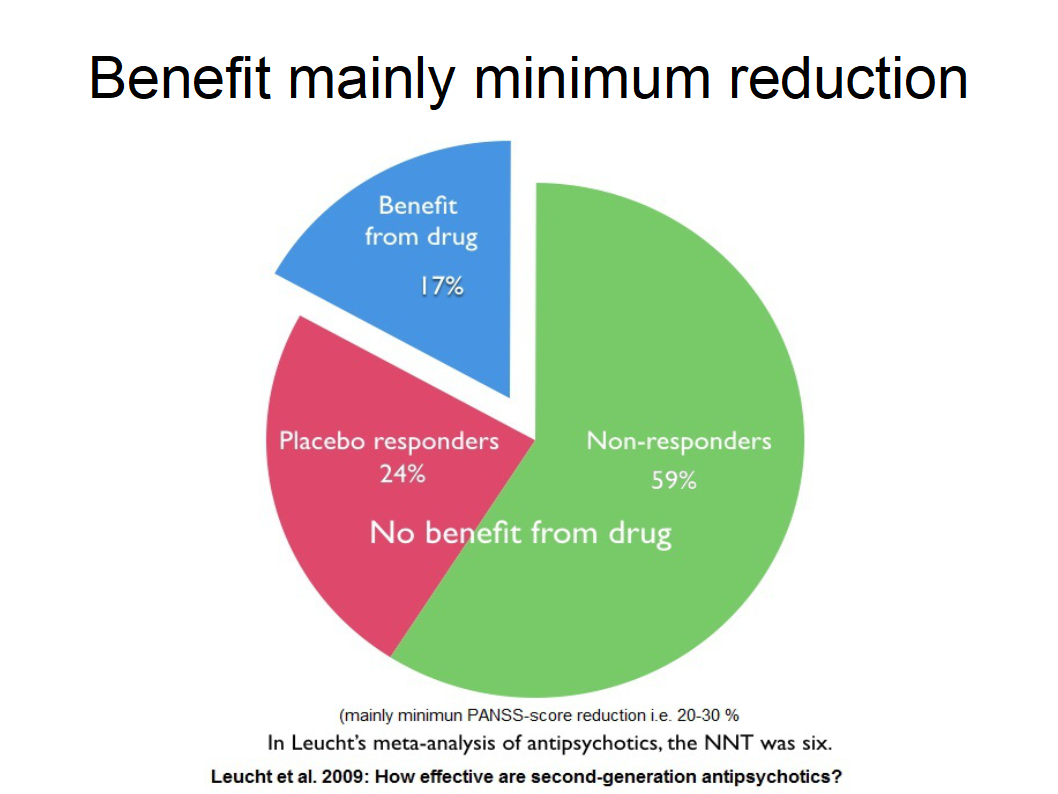
Goff et al. 2017 quotes Leucht et al. 2009 which reads: “The absolute difference (RD) in responder rates was at 18% (41% responded to drug compared with 24% to placebo, number needed to treat=6).” Only 41% and 24% placebo are mentioned but 18% benefit is forgotten. This study is based on minimal symptom-reduction for 2 third of the studies. This is not mentioned.
Leucht et al. 2017 (“Sixty Years of Placebo-Controlled Antipsychotic Drug Trials in Acute Schizophrenia”)6 examined both minimal and good symptom reduction. "Good response" for symptom reduction for acute psychosis was 23% minus 14% placebo, i.e., 9% due to the drug. 91% do not benefit from antipsychotics. The Positive and Negative Syndrome Scale (PANSS) was used to evaluate symptoms.
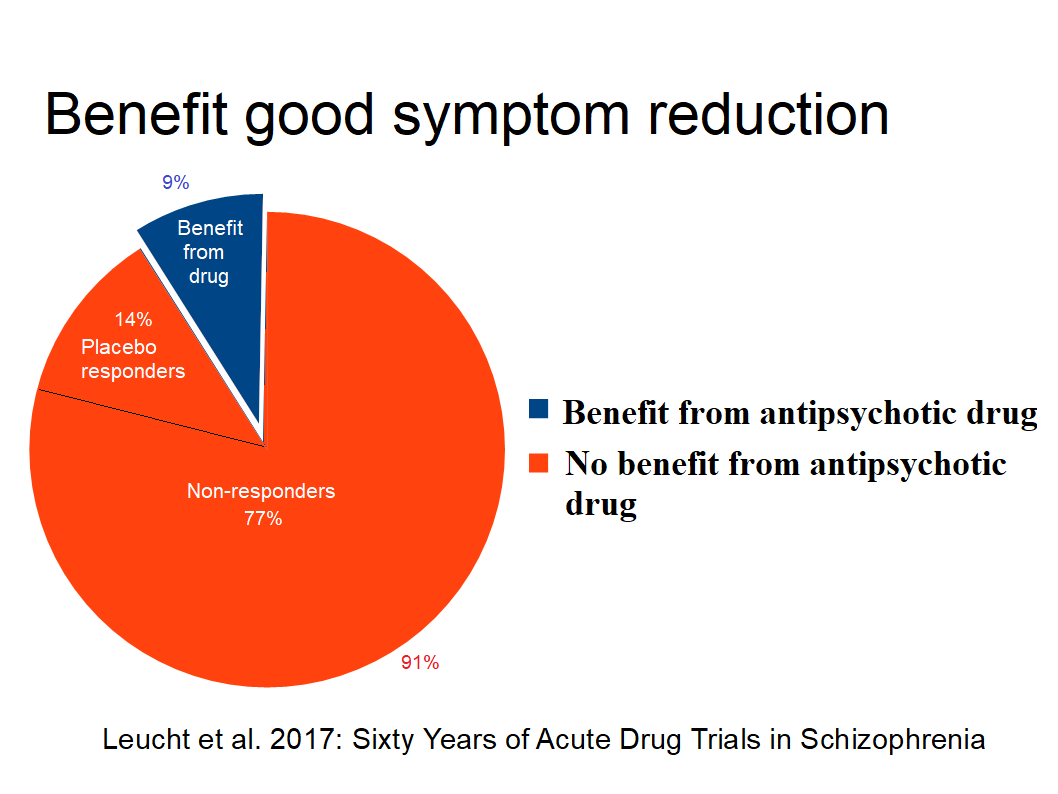
Figure 2: Good acute symptom reduction
WHO's Mental Health Action Plan 2013-2020 is with emphasis on recovery. Both the United States, Canada, New Zealand, Australia, the UK and Ireland are building their national strategies on recovery. There is no evidence that antipsychotics promote "psychosocial functioning, professional functioning, and quality of life" (Buchanan et al 2009 PORT Treatment Recommendations)
Conclusion for acute treatment: 9% of patients treated with antipsychotics benefit with acute good symptom-reduction. However this effect is uncertain due to the lack of medication-naive i.e. wash-out period of placebo group. The aim of treatment according to laws is recovery and symptom-reduction is not necessarily contributing.
For maintenance the summary reads:
The effectiveness of maintenance treatment for prevention of relapse is well established. A subgroup of patients, which may be as large as 20%, may maintain remission or partial remission for extended periods off medication.
Leucht et al. 20127 on relapse prevention is mentioned with NNT 3. However “(N)othing is known about the very long effects of antipsychotics compared to placebo”. Future studies should focus on the long-term outcomes of social inclusion and the long term morbidity is not mentioned.
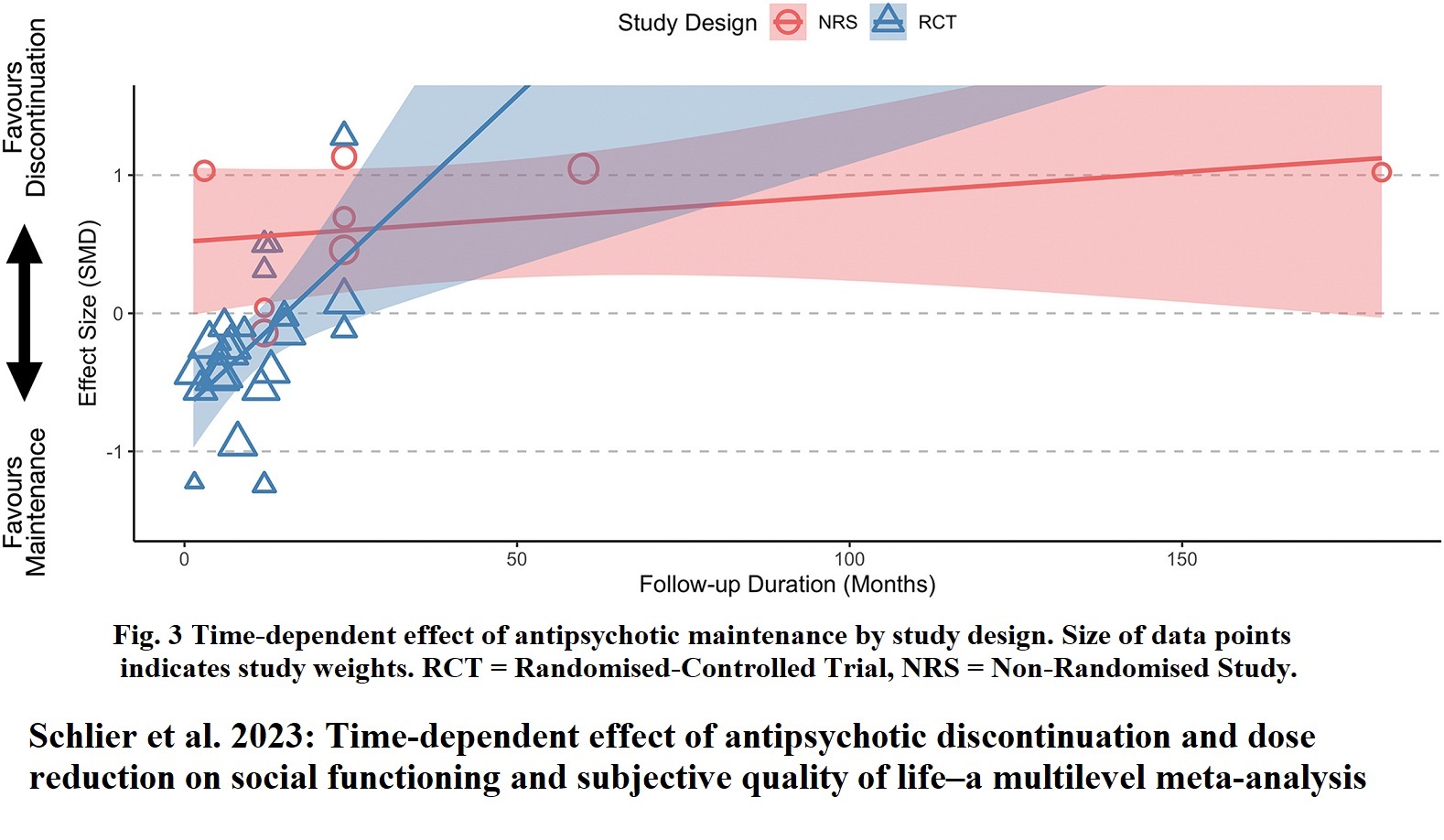
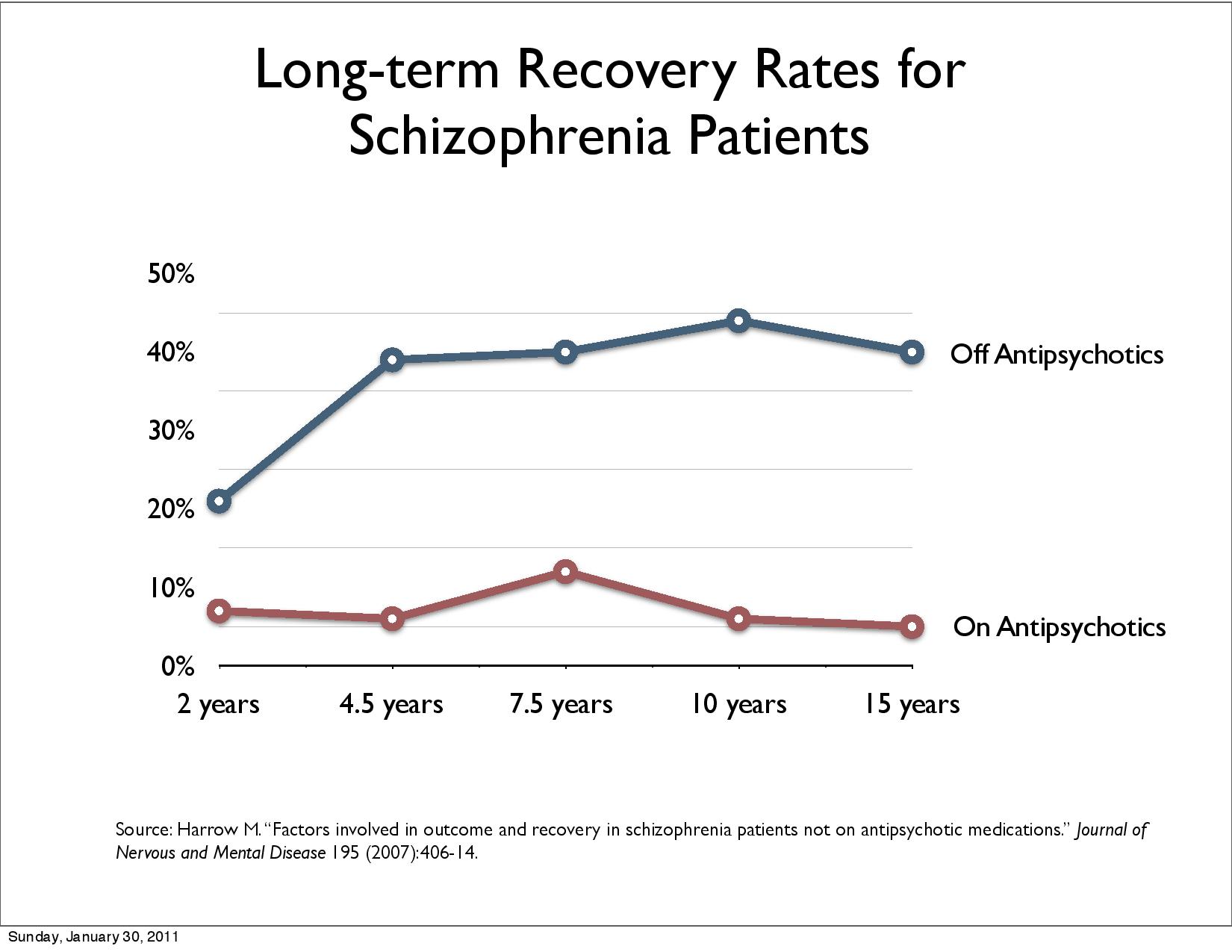
2013, Lex Wunderink8 7 years study shows that patients with reduction/discontinuation are better off i.e. drug reduction/discontinuation gave 40% recovery, and maintenance gave 18% recovery. It is important to see that maintenance effect is time-dependant.
Harrow found seven-fold higher recovery rate for the off-med group remained throughout the study. This can not bee explained by “nonmedicated patients had more favorable premorbid characteristics”. In this study, those with milder disorders who stayed on antipsychotics had worse outcomes than schizophrenia patients who got off the medication.
The Norwegian Institute of Public Health wrote 24 September 2018: “Faith in these drugs was then so great that not a single randomized study was carried out in which a group of patients did not use antipsychotics. There are still no such studies...If you stop taking antipsychotics suddenly, the risk of relapse is great. It is difficult to determine for the individual patient whether the relapse is due to abstinence and what is due to the loss of a possible protective effect of antipsychotics.”
Leucht et al. 2012 Figure 7 shows that maintenance protection against relapse is time-dependant. Schlier et al. 2023 conducted the first meta-analysis pooling the long-term effects of antipsychotic maintenance versus discontinuation on functional recovery in people with schizophrenia spectrum disorders. The result was that the benefit of maintenance disappears after two years. Ceraso et al. 2020 has also found time-dependents.
The
easiest way to avoid possible abstinence effects is not to medicate
so many patients.
Sohler et al. 2015 found in “Weighing the Evidence for Harm from Long-term Treatment with Antipsychotic Medications, A Systematic Review” no evidence for long term treatment: “We believe the pervasive acceptance of this treatment modality has hindered rigorous scientific inquiry that is necessary to ensure evidence-based psychiatric care is being offered.”
This evidence for medicating nearly all is already very weak, but there is no evidence at all for long-term medication.
Bergström et al. 20189 compared Open dialogue patients in northern Finland with all FEP patients in Finland over a period of 19 years. Open dialogue (OD) uses neuroleptics for 20% of patients in the beginning, standard treatment (CG control group) 70%. 97,3 % of the CG get neuroleptics at some point. At the end, 36% of OD patients use neuroleptics, for CG it is 81%.Disability allowance, readmission and patients under treatment halves with OD. Randomisation should guarantee that patients are evenly distributed among groups. This study is based on a “natural randomisation” and the study discusses that the open dialogue area is comparable to the rest of Finland with small discrepancies. Comparison with traditional RTC studies shows advantages of this study:
No selection bias because all patients in both groups are included
At onset only 20.4% of patients are medicated in the Open dialogue area i.e. 80% are antipsychotics naïve and avoids this weakness of traditional RCTs
Disability, readmission, and patients under treatment reflects recovery better than symptom reduction
long-term recovery is covered an area traditional RCTs do not cover
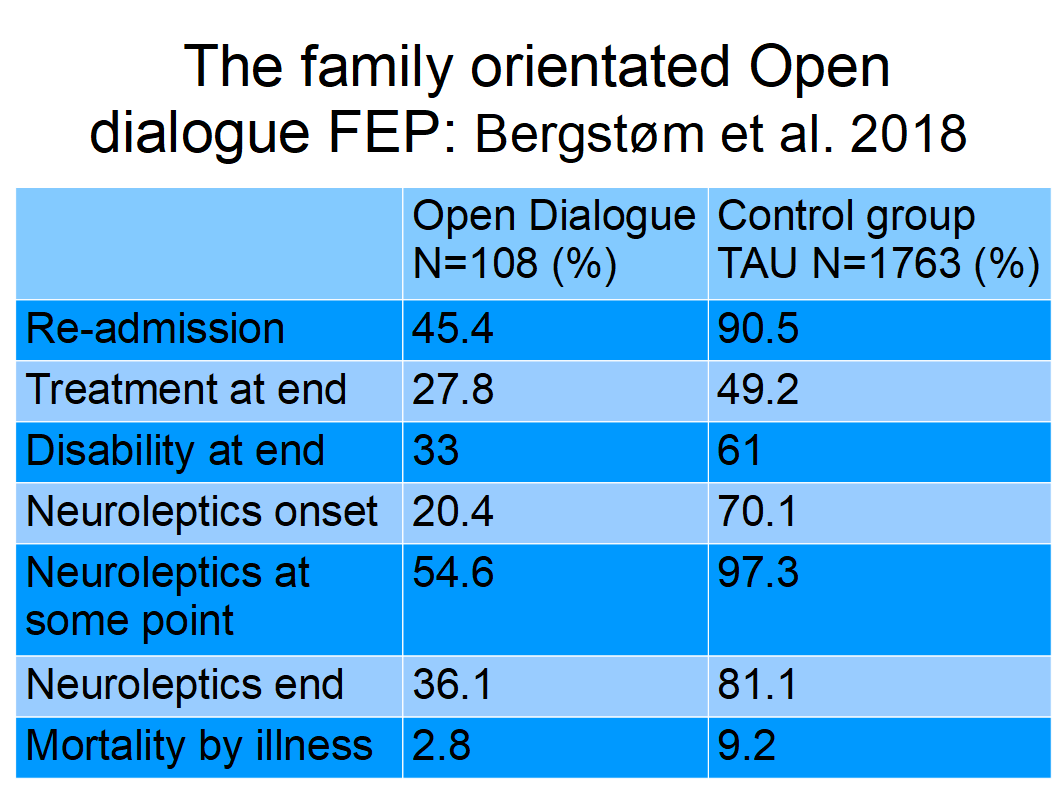
Figure 4: Nineteen–year outcomes: The family-oriented open dialogue approach in the treatment of first-episode psychosis
Conclusion for maintenance treatment: Maintenace studies are unreliable, i.e. the contribution of abstinence effect is not known. Most studies are too short and do not take into account that positive effects seem to last no longer than 2 years.
Due to the low symptom reduction and lack of recovery effect, many patients want to stop taking antipsychotics. This is obviously urgent for non-responders, who have no advantage from antipsychotics, only the disadvantage of side effects. Psychiatric literature stipulates 20% to 30% non-responders. However, Leucht et al. found in 2017 that 79% did not respond with acute good symptom reduction, and 91% had no benefit of drugs. According to Samara et al. 201910 19.8% of patients experience an even symptom increase, approximately half clinically observable. 43% do not respond for cut-off 25% (minimal) and 66,5% for 50% cut-off (good) reduction. The overall percentage of no symptomatic remission was 66.9% .
From patients perspective the wish to stop treatment that does not help seems logical. But psychiatrists are not informed about the magnitude of the problem and underestimate non-responders. Non-conformance of patients is attributed to lack of insight due to illness, negative attitude towards treatment, substance use or abuse, and poor therapeutic alliance.
Lindstrøm et al.11 examined “Patient-rated versus clinician-rated side effects of drug treatment in schizophrenia. Clinical validation of a self-rating version of the UKU Side Effect Rating Scale”. All side effects summed up to 94% of patients. The study found a varying but statistically significant correlation between patient and clinician rated side effects. The highest correlations were found for items belonging to the sub-groups Psychic and Autonomic Side Effects, and the lowest in the subgroup of Neurological Side Effects. Patients reported the side effects more frequently and more severely than the clinicians.
Lacro et al 200212 reported non-adherence rates in schizophrenia range between 40% and 50%, Vega et al. 202113 reported non-adherence was high (58.2%) in the six-month post-discharge period.
Lieberman et al. 201114 stated «The most striking result of the Clinical Antipsychotic Trial of Intervention Effectiveness (CATIE) study, which enrolled almost 1,500 individuals with chronic schizophrenia, was the high rate of treatment discontinuation (up to 74%) over the 18-month period of the trial and the short median time to discontinuation of treatment (about 6 months) in all phases of the trial.». The initial CATIE report 2005 has been cited in the literature over 1,600 times.
Koops et al. 202315: Addressed the evidence to practice gap: “What to Expect From International Antipsychotic Dose Reduction Studies in the Tapering Anti-Psychotics and Evaluating Recovery Consortium?”: «Within the first year of treatment, up to 58% of patients discontinue medication without consulting their professional caregivers».
Due to low effect and many side effects, many patients stop taking antipsychotics, seen as non-adherence by psychiatrists caused by a lack of insight. Many patients want medication-free treatment (Standal 202116) opposed by psychiatrists.
Applying strict requirements «The use of antipsychotics cannot be justified» (Danborg et al. 2019) in the first place. Maintenance for 91% og patients with no benefit of questionable good symtomreduction is not advisable.
Morrison et al. 2020 concludes: «This trial is the first to show that a head-to-head clinical trial comparing psychological intervention, antipsychotics, and their combination is safe in young people with first-episode psychosis..All three regimens were broadly safe and acceptable, with no involuntary hospital admissions and no suggestions that psychological interventions in the absence of antipsychotic medication were detrimental.»
In 2020, there was a sensational study (Francey et al. 2020) with the result that psychosocial treatment alone is no worse than psychosocial treatment with neuroleptics.
There are also good experiences from treatment centers where psychosocial treatment is emphasized and antipsychotics (AP) are used to a small extent, including in the USA Soteria (Calton, Ferriter, Huband, & Spandler, 2007), Finland Open dialogue (Bergström et al., 2018), Denmark OPUS (Wils et al., 2017), Sweden (Cullberg, Levander, Holmqvist, Mattsson, & Wieselgren, 2002) and Norway Basal Exposure Therapy (Hammer, Heggdal, Lillelien, Lilleby, & Fosse, 2018), se Øvernes 2019, Harrow, M. & Jobe, T.H. (2012),
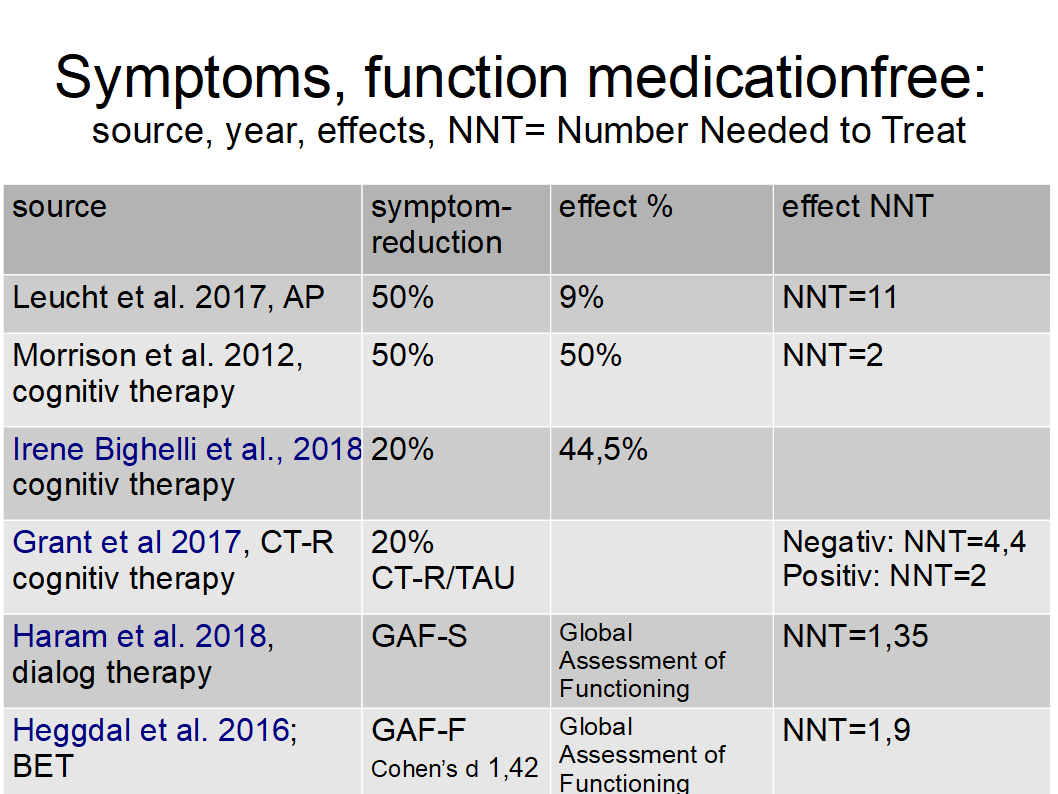
To help one 11 must be medicated with antipsychotics to obtain good reduction of symptoms, while BET and dialogue therapy help one with less than two treated to obtain Global Assessment of Functioning (GAF) which is more relevant for recovery.
Long-term treatment outcomes for the schizophrenia spectrum population were more favorable with patients receiving less medication (Joukamaa et al., 2006; Wunderink et al., 2013; Harrow et al., 2014; Nykänen et al. 2015; Harrow et al., 2017).
That is why the United Nations Special Rapporteur on the right to health Mr. Puras has called for «World needs "revolution" in mental health care» due to "unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist"17 .
WHO18 followed up with the “(n)ew WHO guidance (which) seeks to put an end to human rights violations in mental health care”: "This comprehensive new guidance provides a strong argument for a much faster transition from mental health services that use coercion and focus almost exclusively on the use of medication to manage symptoms of mental health conditions, to a more holistic approach that takes into account the specific circumstances and wishes of the individual and offers a variety of approaches for treatment and support". Compulsory Community Treatment Orders and forced injections of antipsychotics are ineffective and unethical.
In 2011, Germany’s Constitutional Court declared the regulations on coercive treatment in two German states unlawful, which effectively stopped coercive antipsychotic treatment in these parts of Germany. In 2012, Germany’s Federal Supreme Court followed these rulings and extended the ban on coercive antipsychotic treatment across Germany when it found the regulations governing coercive treatment in German guardianship law unconstitutional (Zinkler 201619). Germany was without coercive treatment in psychiatry. This real-world experience proves that it is possible to ban forced treatment. Afterwards, criteria for coercive treatment were narrowed, and procedural safeguards were introduced. In Bavaria, the use of forced drugging was reduced from 2of-8% to 0.5% for inpatients.
Flammer et al.20 reported 2018 that in the German state of Baden-Württemberg 0.6 % of inpatients were affected by forced medication either as an emergency or after a judge's decision in 2016. Coercive medication is rarely used.
Inspired by this success, the head of doctors, Martin Zinkler21 at the Heidenheim Klinik in Germany, suggested “End Coercion in Mental Health Services—Toward a System Based on Support Only”.
The WHO-OHCHR guidance launched October 2023 seeks to improve laws addressing human rights abuses in mental health care (WHO-OHCHR 202322) to support countries in reforming legislation in order to end human rights abuses and increase access to quality mental health care.
“While many countries have sought to reform their laws, policies and services since the adoption of the United Nations Convention on the Rights of Persons with Disabilities in 2006, too few have adopted or amended the relevant laws and policies on the scale needed to end abuses and promote human rights in mental health care.”
One of the reasons is to improve treatment. A fundamental shift is required within the field of mental health. Stigma, discrimination, and other human rights violations continue in mental health care settings. The report identifies the "biomedical model of mental health" as the root of many problems. There is an overreliance on biomedical approaches to treatment options, inpatient services, and care, and little attention given to social determinants and community-based, person-centered interventions. Legislation can help ensure that human rights underpin all actions in the field of mental health.

27.
February 2024: Jeffrey
A. Liebermann answered: Walter thanks for the question. The
answer is emphatically yes.
Treatment-As-Usual (TAU) did not improve patients recovery, mainly due to resistance to giving up excessive medication. Legislators can solve this deadlock by following OHCHR suggestions and remove legal permission for forced drugging. This could promote a shift of paradigm of treatment of schizophrenia towards recovery23.
Rindal. 27. February 2024
Walter Keim

References:
1Standal K, Solbakken OA, Rugkåsa J, Martinsen AR, Halvorsen MS, Abbass A, Heiervang KS. Why Service Users Choose Medication-Free Psychiatric Treatment: A Mixed-Method Study of User Accounts. Patient Prefer Adherence. 2021;15:1647-1660. https://doi.org/10.2147/PPA.S308151
2Dalsbø TK, Dahm, KT, Øvernes, LA, Lauritzen M, Skjelbakken T. [Effectiveness of treatment for psychosis: evidence base for a shared decision-making tool] Rapport 2019. Oslo: Folkehelseinstituttet, [Norwegian Institute of Public Health ] 2019.
3Iversen TSJ, Steen NE, Dieset I, et al. Side effect burden of antipsychotic drugs in real life - Impact of gender and polypharmacy. Prog Neuropsychopharmacol Biol Psychiatry. 2018;82:263-271. doi:10.1016/j.pnpbp.2017.11.004 Nov 7. PMID: 29122637.
4Lindström E, Lewander T, Malm U, Malt UF, Lublin H, Ahlfors UG. Patient-rated versus clinician-rated side effects of drug treatment in schizophrenia. Clinical validation of a self-rating version of the UKU Side Effect Rating Scale (UKU-SERS-Pat). Nord J Psychiatry. 2001;55 Suppl 44:5-69. doi:10.1080/080394801317084428
5Danborg PB, Gøtzsche PC. Benefits and harms of antipsychotic drugs in drug-naïve patients with psychosis: A systematic review. Int J Risk Saf Med. 2019;30(4):193-201. doi:10.3233/JRS-195063
6Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, Samara M, Rabaioli M, Bächer S, Cipriani A, Geddes JR, Salanti G, Davis JM. Sixty Years of Placebo-Controlled Antipsychotic Drug Trials in Acute Schizophrenia: Systematic Review, Bayesian Meta-Analysis, and Meta-Regression of Efficacy Predictors. Am J Psychiatry. 2017 Oct 1;174(10):927-942. doi: 10.1176/appi.ajp.2017.16121358. Epub 2017 May 25. PMID: 28541090.
7Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Davis JM. Maintenance treatment with antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2012 May 16;(5):CD008016. doi: 10.1002/14651858.CD008016.pub2
8Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in Remitted First-Episode Psychosis at 7 Years of Follow-up of an Early Dose Reduction/Discontinuation or Maintenance Treatment Strategy: Long-term Follow-up of a 2-Year Randomized Clinical Trial. JAMA Psychiatry. 2013;70(9):913–920. doi:10.1001/jamapsychiatry.2013.19
9Tomi Bergström, Jaakko Seikkula, Birgitta Alakare, Pirjo Mäki, Päivi Köngäs-Saviaro, Jyri J. Taskila, Asko Tolvanen, Jukka Aaltonen. The family-oriented open dialogue approach in the treatment of first-episode psychosis: Nineteen–year outcomes. Psychiatry Research, Volume 270, 2018, Pages 168-175, ISSN 0165-1781. https://doi.org/10.1016/j.psychres.2018.09.039
10Myrto T Samara, Adriani Nikolakopoulou, Georgia Salanti, and Stefan Leucht. How Many Patients With Schizophrenia Do Not Respond to Antipsychotic Drugs in the Short Term? An Analysis Based on Individual Patient Data From Randomized Controlled Trials. Schizophr Bull. 2019 Apr; 45(3): 639–646. Published online 2018 Jul 2. doi: 10.1093/schbul/sby095
11Lindström E, Lewander T, Malm U, Malt UF, Lublin H, Ahlfors UG. Patient-rated versus clinician-rated side effects of drug treatment in schizophrenia. Clinical validation of a self-rating version of the UKU Side Effect Rating Scale (UKU-SERS-Pat). Nord J Psychiatry. 2001;55 Suppl 44:5-69. doi:10.1080/080394801317084428
12Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication non-adherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892-909. doi:10.4088/jcp.v63n1007
13Dulcinea Vega, Francisco J. Acosta, Pedro Saavedra. Non-adherence after hospital discharge in patients with schizophrenia or schizoaffective disorder: A six-month naturalistic follow-up study. Comprehensive Psychiatry, Volume 108, 2021, 152240, ISSN 0010-440X. https://doi.org/10.1016/j.comppsych.2021.152240
14Jeffrey A. Lieberman, M.D., and T. Scott Stroup. The NIMH-CATIE Schizophrenia Study: What Did We Learn? The American Journal of Psychiatry. Published Online:1 Aug 2011. https://doi.org/10.1176/appi.ajp.2011.11010039
15Sanne Koops, Kelly Allott, Lieuwe de Haan, Eric Chen, Christy Hui, Eoin Killackey, Maria Long, Joanna Moncrieff, Iris Sommer, Anne Emilie Stürup, Lex Wunderink, Marieke Begemann, TAPER international research consortium, Addressing the Evidence to Practice Gap: What to Expect From International Antipsychotic Dose Reduction Studies in the Tapering Anti-Psychotics and Evaluating Recovery Consortium, Schizophrenia Bulletin, 2023;, sbad112, https://doi.org/10.1093/schbul/sbad112
16Standal K, Solbakken OA, Rugkåsa J, Martinsen AR, Halvorsen MS, Abbass A, Heiervang KS. Why Service Users Choose Medication-Free Psychiatric Treatment: A Mixed-Method Study of User Accounts. Patient Prefer Adherence. 2021;15:1647-1660. https://doi.org/10.2147/PPA.S308151
17The United Nations Special Rapporteur on the right to health, Dainius Puras “World needs “revolution” in mental health care – UN rights expert” online publication 06 June 2017. https://www.ohchr.org/en/press-releases/2017/06/world-needs-revolution-mental-health-care-un-rights-expert?LangID=E
18WHO “New WHO guidance seeks to put an end to human rights violations in mental health care” online publication 10 June 2021. https://www.who.int/news/item/10-06-2021-new-who-guidance-seeks-to-put-an-end-to-human-rights-violations-in-mental-health-care
19Zinkler, M. Germany without Coercive Treatment in Psychiatry—A 15 Month Real World Experience. March 2016 Laws 5(1):15. DOI: 10.3390/laws5010015
20Flammer E, Steinert T. [The Case Register for Coercive Measures According to the Law on Assistance for Persons with Mental Diseases of Baden-Wuerttemberg: Conception and First Evaluation]. Psychiatr Prax. 2019;46(2):82-89. doi:10.1055/a-0665-6728
21Zinkler, Martin, and Sebastian von Peter. 2019a. End Coercion in Mental Health Services—Toward a System Based on Support Only. Laws 8: 19.
22WHO-OHCHR launch new guidance to improve laws addressing human rights abuses in mental health care. 9 October 2023. https://www.who.int/news/item/09-10-2023-who-ohchr-launch-new-guidance-to-improve-laws-addressing-human-rights-abuses-in-mental-health-care
23Keim W, 2023. Paradigm Shift to Promote a Revolution of Treatment of Schizophrenia to Achieve Recovery, Medical Research Archives, [online] 11(12). https://doi.org/10.18103/mra.v11i12.4866