[English]
Det standardiserte dødelighetstall eller Standardized Mortality Ratios (SMR) uttrykter et forhold som kvantifiserer økningen i dødeligheten av en studie kohort (f. eks. pasienter) i forhold til den generelle befolkningen.
Shockingly, over the last 5 years, a series of large studies, some looking at national databases, have shown that patients with psychosis are 2 to 3 times more likely to die in any one year than the rest of us. Death is primarily by heart attack or stroke. Being two or three times more likely to be dead may not sound much but other studies point to 15-20 years of lost life.
Patients with schizophrenia are 10 times more likely to be dead at the end of the first year of treatment than they were 100 years ago. There is no other illness in medicine where such a statement could be made.
See Healy et al (2012) Mortality in Schizophrenia.
Healy, D. Harris, M. at el. (2006) Lifetime suicide rates in treated schizophrenia: 1875-1924 and 1994-1998, In Brit J. of Psych, 18, 8, p. 223-228: The suicide rate in schizophrenia between 1875 and 1924 was 20 per 100 000 hospital years, a lifetime rate of less than 0.5%. The suicide rate for all psychoses was 16 per 100 000 hospital years. Current rates of suicide for schizophrenia and other psychoses appear 20-fold higher. CONCLUSIONS: These findings point to an increase in suicide rates for patients with schizophrenia.
I midten av 50-tallet ble nevroleptika / antipsykotika introdusert. I de tre tiårene fra 1950-tallet til 1980-tallet ble selvmord i psykiatriske sykehus tidoblet i Norge (Retterstøl 1988), og økte fra 50 til 400 per 100 000 i veteran (V.A.) sykehus i USA (Farberow 1975). Lignende tendenser er rapportert fra mer enn 8 land (Chart 1: Bowers et al. 2008).
Psykiater Siri Nome har undersøkt dødsfall ved Sandviken psykiatriske sykehus i Bergen. Median-tap i levealder for pasientene som var yngre enn 65 år ved første innleggelse var for menn/kvinner respektive 26,95/23,96 år.
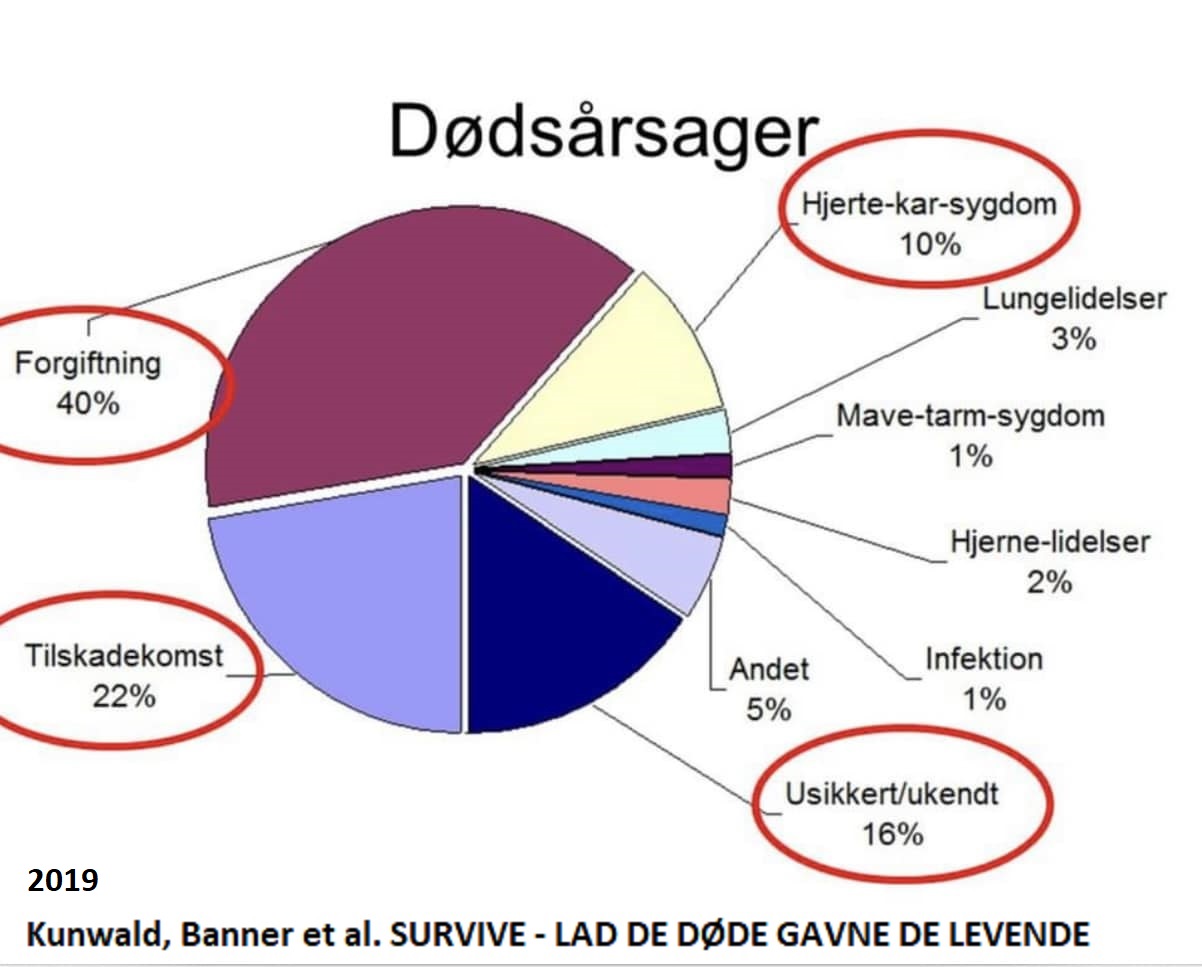
Kunwald, Banner et al. 2019 SURVIVE
- LAD DE DØDE GAVNE DE LEVENDE
Et obduktionsbaseret studie af
årsagerne til tidlig død blandt personer med psykisk sygdom
2022 Institut for Menneskerettigheder. Danmarks
Nationale Menneskerettighedsinstitution
VIDEN
OM TIDLIG DØD I PSYKIATRIEN.
EN UNDERSØGELSE AF, HVORDAN
RETSLÆGELIGE OBDUKTIONER KAN FREMME RETTIGHEDER FOR MENNESKER MED
PSYKISKE LIDELSER
Koncentrationen af psykofarmaka, der kan udløse alvorlige hjerterytmeforstyrrelser, svinger ifølge nyt ph.d.-studie i retskemi voldsomt hos obducerede psykisk syge og er hos nogle op til 20 gange højere end det, der regnes for normale værdier i blodet. Det kan være en kilde til uforklarlige dødsfald, advarer. Dagens Medicin, 15/02/2019.
Resultater for flere
land er "SMR for 1970, 1980 og 1990 var henholdsvis 1,8, 3,0 og
3,2" (John
McGrath et al. 2008), dvs. dødelighetstallet fortsetter å øke.
David
Healy et al. 2012: Mortality in schizophrenia and related
psychoses: data from two cohorts, 1875–1924 and 1994–2010. "Den
mest slående i denne studien er at eliminering av selvmord i
schizofreni ville gjenopprette levetiden til normal." «The
importance of the historical cohort in this study is that it
demonstrates that suicide is not an inherent risk of schizophrenia.
The historical data suggest that there is something about the modern
delivery of care that contributes to suicide as an outcome»
Tiihonens
2009 FIN11 kohort studie har påstått av nevroleptika redusere
dødsrisiko, men er blir motsagt av De
Hert et al. 2010 bl. a. ekskludering av mange dødsfall i
sykehus. «A number of methodological and conceptual issues make the
interpretation of these findings problematic, including incomplete
reporting of data, questionable selection of drug groups and
comparisons, important unmeasured risk factors, inadequate control
for potentially confounding variables, exclusion of deaths occurring
during hospitalization leading to exclusion of 64% of deaths on
current antipsychotics from the analysis, and survivorship bias due
to strong and systematic differences in illness duration across the
treatment groups»
Robert.Whitaker May 2020: Do Antipsychotics Protect Against Early Death? A Review of the Evidence. «In both psychiatric and non-psychiatric patients, the use of antipsychotics doubles the risk of death in comparison to patients who do not take the medications.» The “antipsychotics lengthen lives” research of Jari Tiihonen is flawed in so many ways.
Robert Whitaker October 2020: Viewpoint: do antipsychotics protect against early death? A critical view «These findings (Tiihonen) stand in contrast to studies in non-psychiatric patients that have found that antipsychotics, because of their adverse effects on physical health, increase the risk of early death.»
The Lancet november 2019. Correspondence: Michael P Hengartner, John Read, Joanna Moncrief: «Considering the contradictory evidence that exists, it is incorrect to claim that antipsychotics reduce mortality risk in people with psychotic disorders and we should remain mindful of the possibility that they might increase this risk.»
Dr. Jeff Rubin: Does “Antipsychotic” Treatment Reduce Risk of Death? «To my dismay, after studying the relevant research, I have found that the current psychiatric medical approach for addressing these types of concerns appear to be causing far more harm than good.» Her blir mange studier (f. eks. av Jari Tiihonen) kommentert.«Mens de ble lagt inn på sykehus, var de medisinert, ifølge ett team av forskere som hadde engasjert seg i en lignende studie med det samme datasettet, og mange ble lagt inn på sykehus flere ganger. Hva forskerne egentlig mente med å merke gruppen “ingen antipsykotisk gruppe”, var pasienter som ikke tok dem hver gang de ble løslatt fra sykehuset.»
Weinman et al., 2009: There is some evidence that long-term exposure to antipsychotics increases mortality in schizophrenia. More rigorously designed, prospective studies are urgently needed.
Wahlbeck et al 2011: Redusert levetid for mannlige psykiatriske pasienter var på 2000-tallet 22 år i Danmark, 19 år i Finland og 20 år i Sverige. Dette tilsvarte SMR for levetid-reduksjon av henholdsvis 2,5 for Danmark, 1,8 for Finland og 2,2 for Sverige. SMR for selvmord var 25, 9 og 21, dvs. selvmord er den dominerende årsak. Kvinner har noe lavere tall.
Derfor bør "Antipsykotika brukes mer selektivt, for kortere varighet og med lavest mulig effektiv dose." (Weinmann et al., 2010).
(Norwegian) nationwide open cohort study from 2009 to 2015, including all Norwegians aged 20–79 with schizophrenia and/or substance use disorder registered in any specialized health care setting in Norway, a total of 125,744 individuals: SMR=11.6 for schizophrenia (Ina H. Heiberg et al. 2018).
“Thirty‐one participants (11%) were dead at follow‐up (SMR 11.56; 95% CI: 7.86‐16.42). Sixteen (6%) died by suicide (SMR 46.50, 95% CI: 26.58‐75.51); seven (2.5%) by accidental overdoses or other accidents, and eight (2.8%) from physical illnesses, including three (1%) from cardiovascular illness.” (Ingrid Melle et al. 2017)
“Cognitive behavioural therapy compared to treatment as usual reduced the risk of a new suicide attempt; risk ratio 0.47; 95% confidence interval 0.30–0.73; p = 0.0009; I2 = 57%.” (Peter C Gøtzsche et al. 2017)
I “Suicide in the Age of Prozac” fokuserer Robert Whitaker på inflytelsen av antidepressiva siden 90-årene.
"Personer med alvorlig psykisk lidelse dør opptil 20 år yngre ..." ... "Helse-tjenester bør vurdere et skifte fra fysiske helseovervåkingsstrategier, og i stedet fokusere deres ressurser på primære forebyggende strategier ... Disse inkluderer røykestop (med farmakologisk støtte), diett- og treningsintervensjoner og, hvor det er mulig, for å unngå langvarig bruk av antipsykotika forbundet med uønskede metabolske resultater. "(Athif Ilyas et al., 2017).
PETER C. GØTZSCHE, professor, dr.med., Rigshospitalet gir en oversikt av problemene og hvordan de kan løses:
I KRONIKEN 5. AUG. 2015 oppsummerer i Politikken: Tvang i psykiatrien bør forbydes «(S)amlet set er psykofarmaka den tredjehyppigste dødsårsag i vestlige lande, efter hjerte-kar-sygdomme og kræft».
I 'Dødelig psykiatri og organiseret benægtelse' (2015) skriver P. Gøtzsche: "Jeg mener, vi kan reducere vort nuværende forbrug af psykofarmaka med 98 % og samtidig forbedre folks mentale sundhed og overlevelse."
Peter C. Gøtzsche 10. mars 2017 Dagens Medisin: Psykofarmaka dreper mange
Peter Gøtzsche kommenterer Ulrik Malt sitt innlegg i Aftenposten 21. juni 2019: Antipsykotika øger risikoen for at dø, hvilket er en af grundene til, at patienter med skizofreni lever 20-25 år kortere end andre personer.
Litteratur/Referanser:
Suicides in V.A: hospitals 1950 - 1974: http://wkeim.bplaced.net/files/antipsychotics-Figure-2-1024x768.gif (Farberow NL, Mac Kinnon D (1975) Status of suicide in the veterans administration. Report III ?)
Retterstøl N. (1988) Increasing
Suicide Rate in Scandinavian Psychiatric Hospitals. In: Möller HJ.,
Schmidtke A., Welz R. (eds) Current Issues of Suicidology. Springer,
Berlin, Heidelberg. Suicides per 100000 patients per year in the
psychiatric hospitals in Norway increased from 35 in the period
1950-1954 to 373 in
1980-1984.
https://link.springer.com/chapter/10.1007/978-3-642-73358-1_12
Len Bowers, Henk Nijman, Tumi
Banda 2008. Suicide inside: a literature review on inpatient suicide
https://www.kcl.ac.uk/ioppn/depts/hspr/archive/mhn/projects/litreview/LitRevSuicide.pdf
“Reported rates of inpatient suicide varied by all three
commonly used denominators – admissions, population and total
number of suicides – indicating that such figures are influenced
by social and service organisation factors. Rates in some countries
have risen during the latter half of the 20th Century. The reasons
for this are unknown”
Ina H. Heiberg et al. 2018. Total and cause-specific standardized mortality ratios in patients with schizophrenia and/or substance use disorder. “We performed a (Norwegian) nationwide open cohort study from 2009 to 2015, including all Norwegians aged 20–79 with schizophrenia and/or substance use disorder registered in any specialized health care setting in Norway, a total of 125,744 individuals. The SMRs were 4.9 (95% CI 4.7–5.1) for all schizophrenia patients, 4.4 (95% CI 4.2–4.6) in patients with schizophrenia without substance use disorder, 6.6 (95% CI 6.5–6.8) in patients with substance use disorder only, and 7.4 (95% CI 7.0–8.2) in patients with both schizophrenia and substance use disorder. ” https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0202028&type=printable
Wahlbeck, K., Westman, J.,
Nordentoft, M., Gissler, M., & Laursen, T. (2011). Outcomes of
Nordic mental health systems: Life expectancy of patients with
mental disorders. British Journal of Psychiatry, 199(6), 453-458.
doi:10.1192/bjp.bp.110.085100
https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/outcomes-of-nordic-mental-health-systems-life-expectancy-of-patients-with-mental-disorders/D9769E301E9C238CA3B43E21E1913DF7
“Our results show that deinstitutionalisation can be
implemented while maintaining or even improving the life expectancy
of people with mental disorders across countries. In spite of the
transition of mental health services, however, the life expectancy
gap has remained largely unchanged over 20 years, and major health
inequalities persist between people with mental disorders and the
rest of the population.”
Psychiatry Ignores an Elephant in the Room By Peter Gøtzsche, MD September 21, 2017. https://www.madinamerica.com/2017/09/psychiatry-ignores-elephant-room/ “Large cohort studies of people with a first-episode psychosis provide a unique opportunity for finding out why so many young people with schizophrenia spectrum disorders die at a young age. However, it seems that those psychiatrists who have access to the mortality data generally do not want the facts to come out. In published cohort studies, there is virtually always too little information or no information at all about the causes of death.” Follow-up 16 February 2018, 8 March 2018, October 11, 2018 (Gøtzsche expelled from COCHRANE).
Ingrid Melle et al. 2017. Causes and predictors of premature death in first‐episode schizophrenia spectrum disorders. https://onlinelibrary.wiley.com/doi/full/10.1002/wps.20431 “Thirty‐one participants (11%) were dead at follow‐up (SMR 11.56; 95% CI: 7.86‐16.42). Sixteen (6%) died by suicide (SMR 46.50, 95% CI: 26.58‐75.51); seven (2.5%) by accidental overdoses or other accidents, and eight (2.8%) from physical illnesses, including three (1%) from cardiovascular illness.”
October 11, 2018 Mad in America. The Cochrane Collaboration Has Failed Us All. By Robert Whitaker: “There is now a scientific trail to follow in this exchange. The lead author of the TIPS study doesn’t respond to Gøtzsche’s inquiry (bad science); the editor of the journal that published the article won’t publish a letter raising the question about the deaths (bad science); and the research director for one of the funders doesn’t respond to the question either (more bad science). Instead, he writes a letter of complaint to Cochrane CEO Mark Wilson, stating that since Gøtzsche has a relationship with the Hearing Voices group, he isn’t going to believe anything that the Cochrane Collaboration publishes about mental illness!”
Sukanta Saha et al. 2007: A Systematic Review of Mortality in Schizophrenia: The median SMR for those diagnosed in the 1970s, 1980s, and 1990s were 1.84, 2.98, and 3.20, respectively. The higher the SMR, the higher the rate of mortality.
John McGrath et al. 2008:
Schizophrenia: A Concise Overview of Incidence, Prevalence, and
Mortality https://academic.oup.com/epirev/article/30/1/67/621138
The SMRs for all-cause mortality significantly increased over
recent decades (p = 0.03): the median SMRs for the 1970s, 1980s, and
1990s were 1.8, 3.0, and 3.2, respectively.
Risks of all-cause and suicide
mortality in mental disorders: a meta-review
Edward Chesney et
al. 2014 https://onlinelibrary.wiley.com/doi/full/10.1002/wps.20128
The reduction in life expectancy associated with moderate to
heavy smoking ranged from 8 to 10 years. This range is similar to
that reported for a single depressive episode or recurrent
depressive disorder (7-11 years), but lower than that associated
with substance use (9-24 years), personality disorders (13-22
years), schizophrenia (10-0 years), and bipolar disorder (9-20
years) (Table 3).
Influence of
antipsychotics on mortality in schizophrenia: systematic
review.Weinman
et al.: Schizophr Res. 2009 Aug;113(1):1-11. doi:
10.1016/j.schres.2009.05.018. Epub 2009 Jun 12.
https://www.ncbi.nlm.nih.gov/pubmed/19524406
There is some evidence that long-term exposure to antipsychotics
increases mortality in schizophrenia. More rigorously designed,
prospective studies are urgently needed.
Antipsychotic medication,
mortality and neurodegeneration: The need for more selective use and
lower doses
February 2010(Psychosis) Psychological, Social and
Integrative Approaches 2(1):50-69
DOI: 10.1080/17522430903501999
Stefan Weinmann Volkmar Aderhold:
https://www.researchgate.net/publication/233138682_Antipsychotic_medication_mortality_and_neurodegeneration_The_need_for_more_selective_use_and_lower_doses
"Antipsychotics should be used more selectively, for
shorter durations and with lowest possible effective dose."
Meta-analysis October 2007: A
Systematic Review of Mortality in Schizophrenia Is the Differential
Mortality Gap Worsening Over Time?
Sukanta Saha et al.
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/210034
"With respect to mortality, a substantial gap exists
between the health of people with schizophrenia and the general
community. This differential mortality gap has worsened in recent
decades. In light of the potential for second-generation
antipsychotic medications to further adversely influence mortality
rates in the decades to come, optimizing the general health of
people with schizophrenia warrants urgent attention."
"People
with schizophrenia have a substantially increased risk of death
compared with the general population. Overall, people with
schizophrenia have 2.5 times the risk of dying. This review was able
to extract data from 37 studies that were conducted in 25 countries.
As predicted, the distribution of all-cause SMRs showed prominent
variability.
Confirming the hypothesis that the relative
mortality risk associated with schizophrenia is increasing, we found
that SMRs have increased in a linear fashion during the 3 decades
examined in this study. It is now widely acknowledged that
schizophrenia contributes substantially to the global burden of
disease. It is also well known that schizophrenia is associated with
elevated suicide rates."
Schizophrenia, neuroleptic
medication and mortality.
Joukamaa M et al. 2006
https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/schizophrenia-neuroleptic-medication-and-mortality/713F6B46E0A34BA1203761015F18684B
"The number of neuroleptics used at the time of the
baseline survey showed a graded relation to mortality. Adjusted for
age, gender, somatic diseases and other potential risk factors for
premature death, the relative risk was 2.50 (95% CI1.46–4.30) per
increment of one neuroleptic."
Mortality in schizophrenia and
related psychoses: data from two cohorts, 1875–1924 and 1994–2010
David Healy et al 2012:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3488735/
"We found a 10-year survival probability of 75% in the
historical cohort and a 90% survival probability in the contemporary
cohort with a fourfold increase in standardised death rates in
schizophrenia and related psychoses in both historical and
contemporary periods. Suicide is the commonest cause of death in
schizophrenia in the contemporary period (SMR 35), while
tuberculosis was the commonest cause historically (SMR 9). In the
contemporary data, deaths from cardiovascular causes arise in the
elderly and deaths from suicide in the young.
The most striking
figure in this study is that eliminating suicide in schizophrenia
would restore life expectancy to normal."
Increasing mortality in
schizophrenia: Are women at particular risk? A follow-up of 1111
patients admitted during 1980–2006 in Northern Norway
Anne
Høye et al. 2011:
https://helse-nord.no/Documents/SKDE/SKDE%20Artikler/Increasing%20mortality%20in%20schizophrenia,%20are%20women%20at%20particular%20risk%20(2011).pdf
"In Norway, mortality of patients with mental illness has
been reported
regularly since 1916 (Ødegård, 1936, 1951, 1952;
Ødegård, 1967;
Saugstad and Ødegård, 1979,1985; Hansen et
al., 1997). A previous
study based on the case register of the
University Hospital of North
Norway with follow-up 1980–1992
(Hansen et al., 2001) documented
increase in SMRs compared to
earlier periods, especially high for men...
Our study confirms
the persisting mortality gap between patients
with schizophrenia
and the general population over a period of 27 years,
with a
tendency of increasing SMRs."
Athif Ilyas et al. 2017. Improving
life expectancy in people with serious mental illness: Should we
place more emphasis on primary
prevention?https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/improving-life-expectancy-in-people-with-serious-mental-illness-should-we-place-more-emphasis-on-primary-prevention/5BA82EA9FBBA0E932478CDC4AF6B4601/core-reader
“People with serious mental illness die up to 20 years younger
because of preventable physical disorders” … “Healthcare
services should consider a shift away from physical health
monitoring strategies and instead focus their resources on primary
prevention strategies that are provided to all people with serious
mental illness from the moment they first present to mental
healthcare services. These include assertive smoking cessation (with
pharmacological support), diet and exercise interventions and where
possible, to avoid long-term prescription of antipsychotics
associated with adverse metabolic outcomes.”
Dr. Jeff Rubin: Does “Antipsychotic” Treatment Reduce Risk of Death? «To my dismay, after studying the relevant research, I have found that the current psychiatric medical approach for addressing these types of concerns appear to be causing far more harm than good.»
.