«A
Guide to Minimal Use of Neuroleptics: Why and How by Volkmar
Aderhold, MD and Peter Stastny, MD, June 2015
Rethinking
Antipsychotics(pdf) video Robert
Whitaker, February 2017
Open
Letter to US National
Institutes of Health, UK
National Institute for Health Research
Norwegian
Psychiatric Society (Npf), TIPS,
UiO: NORMENT:
Norwegian Centre for Mental Disorders Research, OUS
Section for Treatment Research, Norwegian
Institute of Public Health, TIPS
early detection in psychosis
Copy:
Ingrid
Melle, Jan Olav Johannessen, Health
directorate, Kim
T. Mueser, Donald
C. Goff, Peter Falkai, Wolfgang Fleischhacker, Ragy R. Girgis, Rene
M. Kahn, Hiroyuki Uchida, Jingping Zhao, Jeffrey A. Lieberman,
Jari Tiihonen
Current treatment recommendations are based on neuroleptics for symptom reduction offered to all patients. However focus is shifting from symptom relieve to recovery getting more attention. Bergström et al. 2018 falsifies treatment as usual. Studies to identify the contribution of elements of alternatives that achieve very good treatment results is suggested.
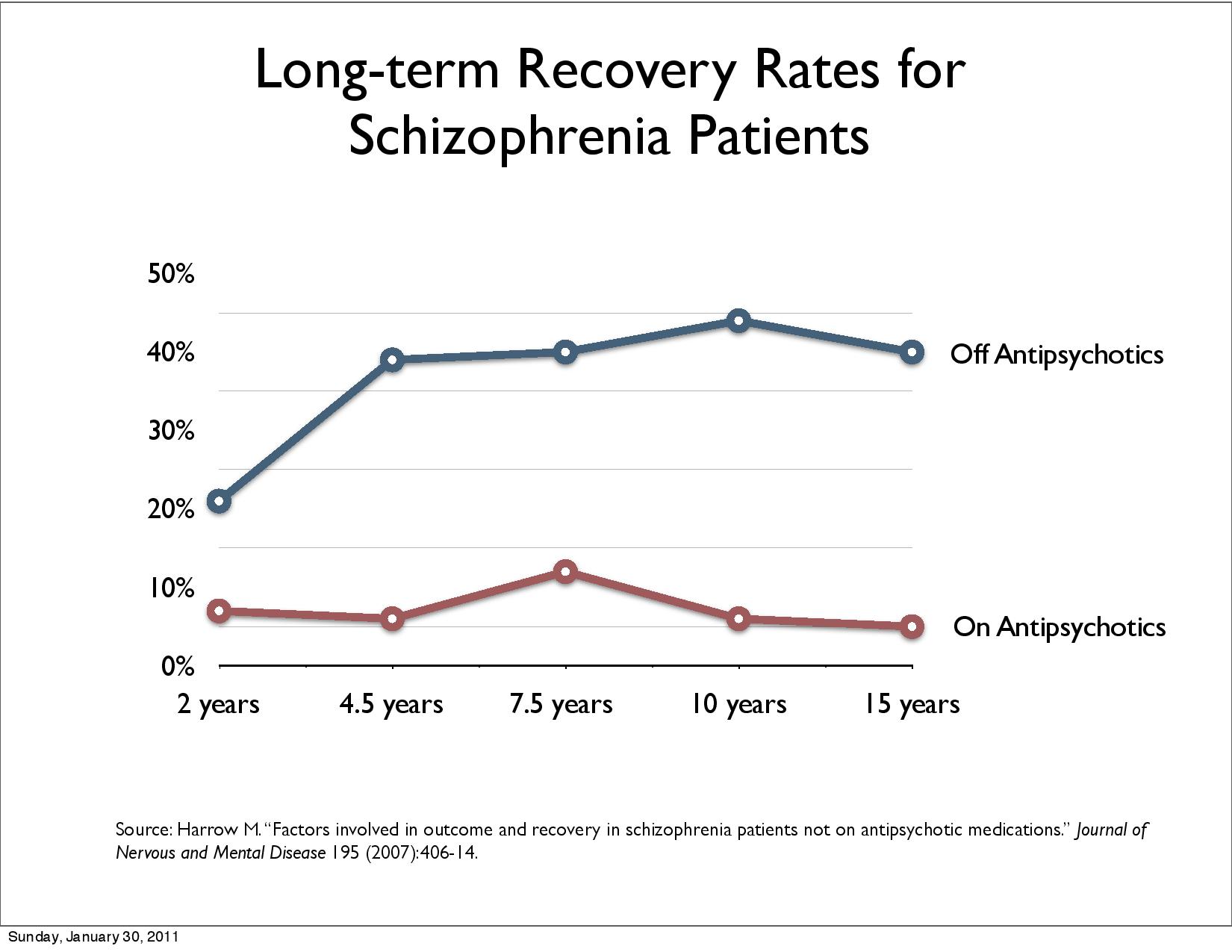
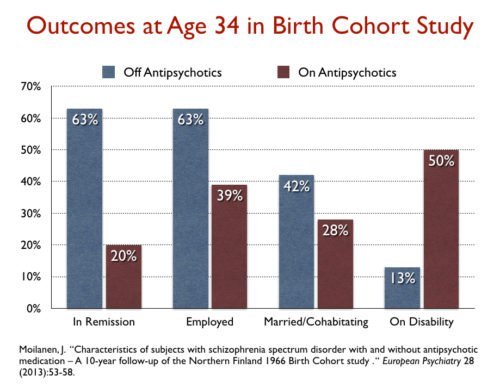
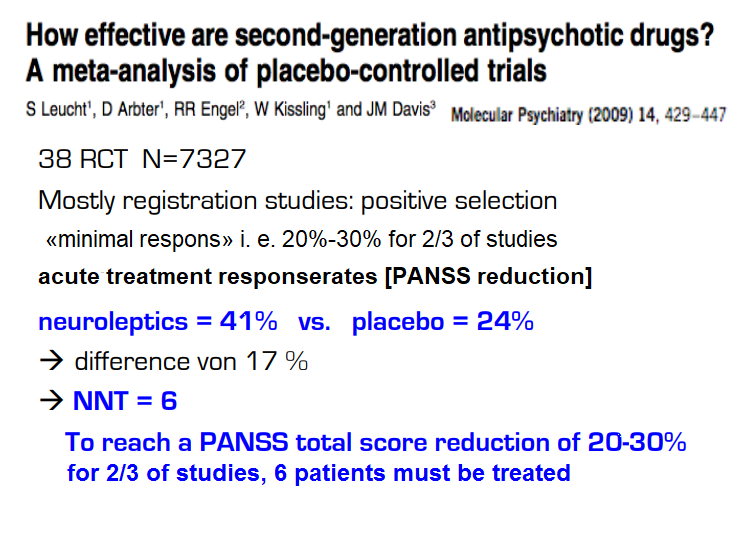
Neuroleptics are used to ease symptoms (Leucht et al 2009: NNT=6) and to prevent relapse (Leucht et al 2012: NNT=3) with evidence at the beginning of the psychosis for a minority of patients. No antipsykotic-naive patients, derfor withdrawl effect. 50,4 % employed in placebo group but in maintenance group 48,4 %.. There is no evidence that antipsychotics promote "psychosocial functioning, professional functioning, and quality of life" (Buchanan et al 2009 PORT Treatment Recommendations). Bjornestad, Larsen et al. 2017 admit that evidence of long-term maintenance medication is missing: "Due to the lacking long-term evidence base (Sohler et al. 2016) ..." Current use of neuroleptics has been criticised (4,6,7). Studies show the advantage of a shift to lower doses for fewer patients over a shorter period of time.
Recovery is used in several meanings and has gained attention and has now become mainstream. The Norwegian Government's Strategy for Good Mental Health (2017-2022) "Mastering Life" is based on WHO's Action Plan 2013-2020 and The European Mental Health Action Plan 2013-2020 and EU JOINT ACTION 2016. Both the United States, Canada, New Zealand, Australia, the UK and Ireland are building their national strategies on recovery. The Norwegian Mental Health Expansion Plan mentions the needs of the user/patient as a starting point, "mastering one's own life", "successful return to working life" and "entering into a social relationship with family and friends" (Ottar Ness 2015).
For social functioning Ceraso et al. 2020 found a maintenance effect of NNT 7 and time-dependence. For more then 2 years to terminate medication is more preferable than maintenance (Schlier et al. 2023).
Recovery rates decreased: «17.7% in studies between 1941 and 1955, 16.9% in 1956–1975, 9.9% in 1976–1995, and 6.0% in studies after 1996» according to Jaaskelainen et al. 2013. Open dialogue quadrupled recovery, reduces schizophrenia per year to one tenth and disability benefit / illness decreases to one third in naturalistic studies (3,5). The evidence in support of OD has been criticised being of low quality, and randomized controlled trials are required to draw further conclusions.
Tomi Bergström, Jaakko Seikkula et al. 2018 (1) compare FEP Open dialogue patients with all FEP patients in Finland over a period of 19 years. Open dialogue (OD) uses neuroleptics for 20% of patients in the beginning, standard treatment (CG control group) 70%. 97,3 % of the CG get neuroleptics at some point. At the end 36% of OD patients use neuroleptics, for CG it is 81%. Disability allowance, readmission and patients under treatment halves with OD, reflecting better recovery.
This register study reflects reality/facts about Finland on national level. Treatment as usual is falsified as the most effective treatment. RCTs could give further information which of Open dialogues approaches e. g. reduction of antipsychotic medication, immediate help within 24 hours, social network perspective, dialogue etc. contributes to the good treatment results.
Scientific studies can only explain reality not disprove. Respect of reality could considerable improve treatment and health of patients. Therefore I have asked Norwegian research institutions in 2018 to do further studies: “Paradigm shift: Can Open dialogue achieve quadruple recovery rate, reduce schizophrenia per year to one tenth and disability allowance/sickness is reduced to one third?
The United Nations Special Rapporteur on the right to health Mr. Pūras has called for «World needs “revolution” in mental health care» to «enable a long overdue shift to a rights-based approach».“There is now unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist” Mr. Pūras said.
In order to make studies possible psychiatrists respect of reality should be strengthened. See comments on psychiatrists reflections on medication-free program: https://www.researchgate.net/publication/330738021_Psychiatrists'_reflections_on_a_medication-free_program_for_patients_with_psychosis/comments
Open dialogue medicates less than halve of patients. Medication free treatment (2,4) beds cover about 60 beds of 4000 beds in Norway. The impact on national level is very small looking at how few additional patients get medication-free treatment.
Economic consequence: In the year 2012 there where «8399 individuals with schizophrenia» in Norway. Total cost was USD 890413045.- (Prevalence, Employment Rate, and Cost of Schizophrenia in a High-Income Welfare Society: A Population-Based Study Using Comprehensive Health and Welfare Registers. October 2015 Schizophrenia Bulletin DOI: 10.1093/schbul/sbv141). Would cutting down medication to half cut in half costs and reduce suffering of patients?
Walter Keim, Rindal, 9. February 2019
Project ODDESSI stands for Open Dialogue (OD): Development and Evaluation of a Social Network Intervention for Severe Mental Illness and is funded by the National Institute of Health Research (NIHR) and managed by North East London NHS Foundation Trust (NELFT). The study will run from 2017-2022. (December 2018 newsletter)
The History of the Open Dialogue Approach in the United States. Presented at the World Open Dialogue Conference, Tokyo and Kyoto, Japan, February 2019.
International website for the Open Dialogue approach: https://open-dialogue.net
The Institute for Dialogic Practice, Northampton MA
Follow-up: 5. May 2019: Researchgate Comment: Suggestion of further research with focus on recovery
Reference:
Bergström et al. 2018: The family-oriented Open Dialogue approach in the treatment of first-episode psychosis nineteen-year outcomes: https://www.researchgate.net/publication/327739553_The_family-oriented_Open_Dialogue_approach_in_the_treatment_of_first-episode_psychosis_nineteen-year_outcomes
Robert Whitaker - May 21, 2017. Psychiatry Defends Its Antipsychotics: A Case Study of Institutional Corruption
Jaakko Seikkula - 7 Principles of Open Dialogue - DK 3 - Roskilde- August 29, 2014: 3. http://wkeim.bplaced.net/files/Seikkula2014.pdf
Sami Timimi. Tidsskr Nor Legeforen 2017 137:421 DOI: 10.4045/tidsskr.17.0240 The option of drug-free/drug withdrawal is the minimum that all http://tidsskriftet.no/2017/04/kommentar/option-drug-freedrug-withdrawal-minimum-all
Scientific Symposium. Pharmaceuticals – risks and alternatives. The 15th of October 2016 in Gothenburg, Sweden. Jaakko Seikkula, Professor of Psychotherapy, Clinical Psychologist, Finland. Naturalistic study designs for developing the system to reduced medication http://extendedroom.org/en/scientific-symposium/
Professor, Doctor of Medical Science, Peter C. Gøtzsche The third leading cause of death after heart disease and cancer?: http://cepuk.org/2015/05/13/third-leading-cause-death-heart-disease-cancer-experts-debate-harmful-effects-psychiatric-medications/ (in Danish: http://www.deadlymedicines.dk/wp-content/uploads/2015/09/Diagnoser_kap-7.pdf
Professor PETER C. GØTZSCHE: Deadly Psychiatry and Organised Denial (pdf). https://www.amazon.com/Deadly-Psychiatry-Organised-Denial-Gotzsche-ebook/dp/B014SO7GHS
Robert Whitaker, February 2017: Rethinking Antipsychotics Recovery Rates and Long-term Outcomes for Unmedicated Patients with Schizophrenia Spectrum Disorders (pdf)
Can Open dialogue achieve quadruple recovery
rate, reduce schizophrenia per year to one tenth and disability
allowance/sickness is reduced to one
third?
http://wkeim.bplaced.net/files/recovery-en.html
A Critical Literature Review of the Direct, Adverse Effects of Neuroleptics (also known as antipsychotics). Essential Information for Mental Health Consumers, Carers, Families, Supporters and Clinicians: https://nmhccf.org.au/sites/default/files/docs/nmhccf_-_clr_-_web_accessible_version_-_final_-_august_2017_0.pdf
Peter C Gøtzsche 10 January 2018 Psychiatry is a disaster area in healthcare that we need to focus on (BMJ 2018;360:k9) http://www.bmj.com/content/360/bmj.k9/rr-15
Robert Whitaker 2015: Antipsychotics/Schizophrenia: Antipsychotic Drugs and Chronic Illness. A. The Chronicity Problem Becomes Apparent (1960s-1970s) https://www.madinamerica.com/mia-manual/antipsychoticsschizophrenia/
Tomi Bergström, Jaakko Seikkula et al. 2018: The family-oriented open dialogue approach in the treatment of first-episode psychosis: Nineteen–year outcomes. Psychiatry Research Volume 270, December 2018, Pages 168-175: https://authors.elsevier.com/a/1XmgRbZg70VfA
Results of long-term use of antipsychotic drugs: