The United Nations Special Rapporteur on the right to health Mr. Pūras has called for «World needs “revolution” in mental health care». “There is now unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist”
Open
Letter to Donald
C. Goff, Peter Falkai, Wolfgang Fleischhacker, Ragy R. Girgis, Rene
M. Kahn, Hiroyuki Uchida, Jingping Zhao, Jeffrey A. Lieberman,
Kim
T. Mueser, US National
Institutes of Health
Copy: UK
National Institute for Health Research, Norwegian
Psychiatric Society (Npf), TIPS,
UiO: NORMENT:
Norwegian Centre for Mental Disorders Research, OUS
Section for Treatment Research, TIPS
early detection in psychosis, Ingrid
Melle, Jan Olav Johannessen, Erik
Johnsen, Health
directorate, Norwegian
Institute of Public Health
I appreciate your constructive contribution: "Strategies for treatment discontinuation or alternative nonpharmacologic treatment approaches may benefit a subgroup of patients ... More research is needed to determine whether some individuals may respond to alternative pharmacologic or nonpharmacologic treatments for a first episode of psychosis..." (Goff et al. 2017: The Long-Term Effects of Antipsychotic Medication on Clinical Course in Schizophrenia).
Based on:
size of antipsychotics effects,
increasing focus on recovery
falsification of current paradigm (Treatment as usual) i. e. recommendation that all individuals with new-onset schizophrenia should receive acute and maintenance antipsychotic treatment
further research is suggested with focus on recovery.
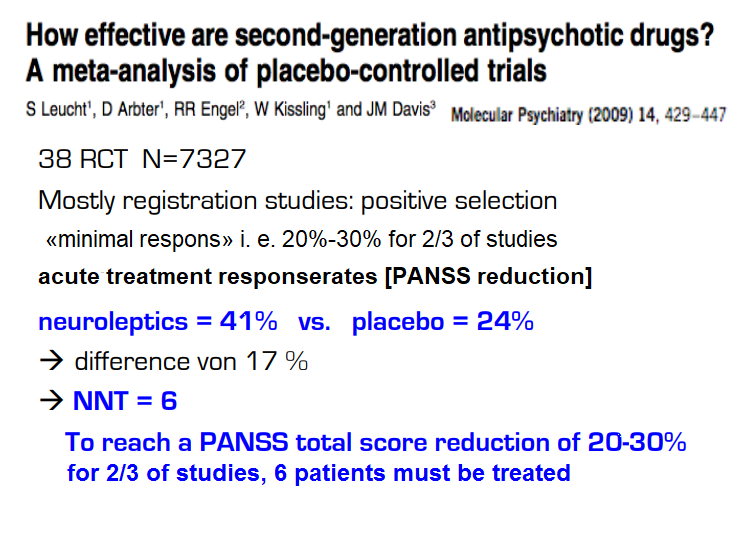
Antipsychotics are used to ease symptoms (Leucht et al 2009: NNT=6) and to prevent relapse (Leucht et al 2012: NNT=3) with evidence at the beginning of the psychosis for a minority of patients. There is no evidence that antipsychotics promote "psychosocial functioning, professional functioning, and quality of life" (Buchanan et al 2009 PORT Treatment Recommendations). Bjornestad, Larsen et al. 2017 admit that evidence of long-term maintenance medication is missing: "Due to the lacking long-term evidence base (Sohler et al. 2016) ..." Current use of neuroleptics has been criticised. Studies show the advantage of a shift to minimal doses for fewer patients over a shorter period of time.
Recovery is used in several meanings and has gained attention and has now become mainstream. Both the United States, Canada, New Zealand, Australia, the UK and Ireland are building their national strategies on recovery. The Norwegian Government's Strategy for Good Mental Health (2017-2022) "Mastering Life" is based on WHO's Action Plan 2013-2020 and The European Mental Health Action Plan 2013-2020 and EU JOINT ACTION 2016. The Norwegian Mental Health Expansion Plan mentions the needs of the user/patient as a starting point, "mastering one's own life", "successful return to working life" and "entering into a social relationship with family and friends" (Ottar Ness 2015). Recovery rates decreased: «17.7% in studies between 1941 and 1955, 16.9% in 1956–1975, 9.9% in 1976–1995, and 6.0% in studies after 1996» according to Jaaskelainen et al. 2013.
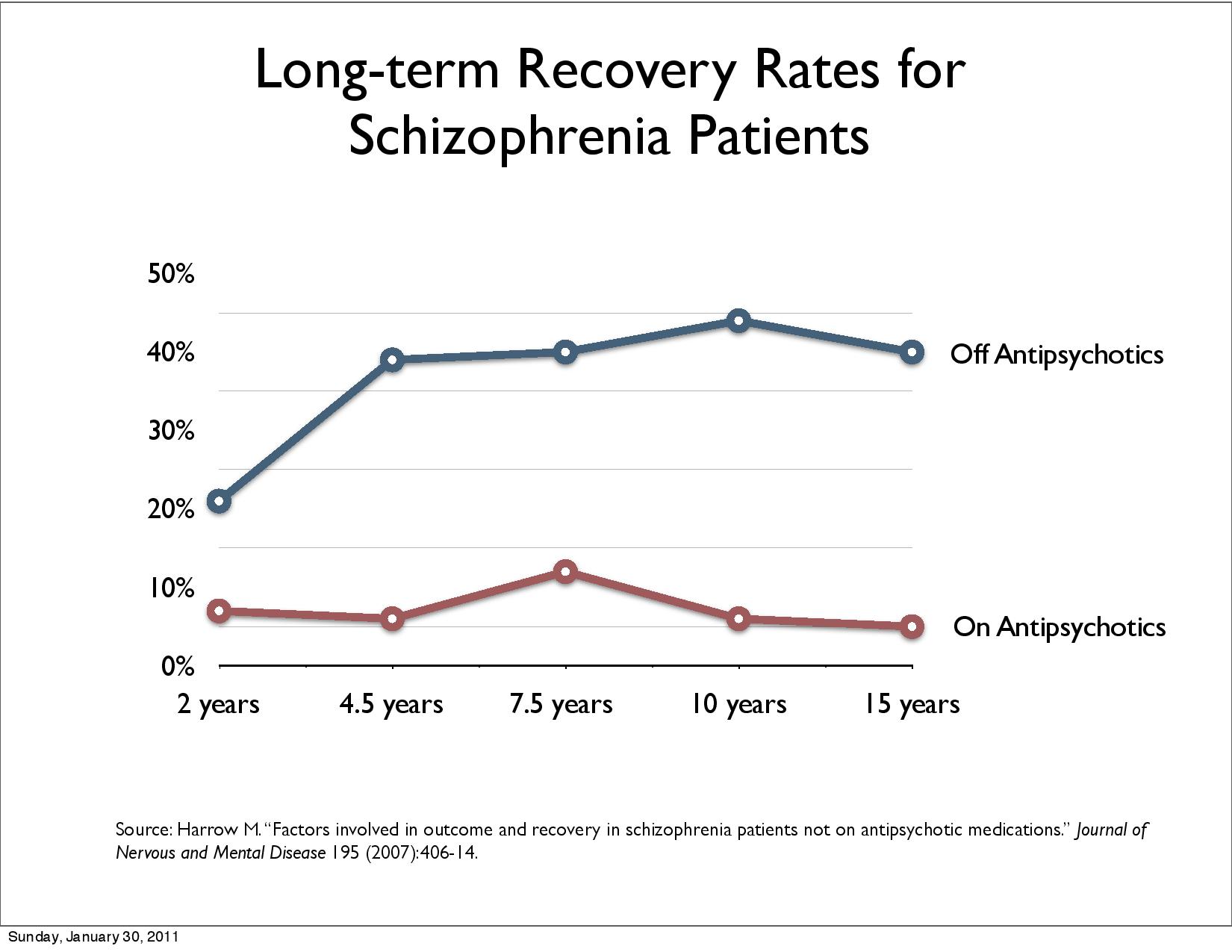
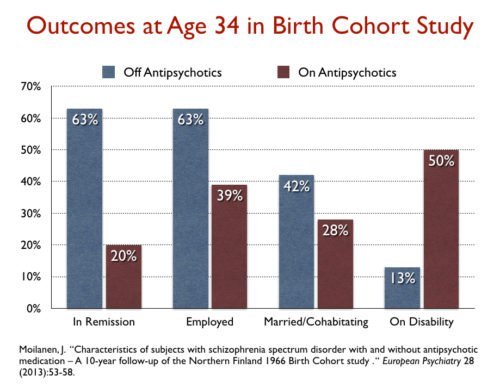
Harrow et al. 2007, Jääskeläinen et al. 2013, Harrow & Jobe (2017), Wunderink et al 2013, Wunderink 2019 look at recovery.
Naturalistic studies of Open dialogue reported good outcomes looking at recovery, reduces schizophrenia per year and reduced disability benefit. The evidence in support of OD has been criticised being of low quality, and randomized controlled trials are required to draw further conclusions.
Tomi Bergström, Jaakko Seikkula et al. 2018 (1) compare FEP Open dialogue patients with all FEP patients in Finland over a period of 19 years. Open dialogue (OD) uses neuroleptics for 20% of patients in the beginning, standard treatment (CG control group) 70%. 97,3 % of the CG get neuroleptics at some point. At the end 36% of OD patients use neuroleptics, for CG it is 81%. Disability allowance, readmission and patients under treatment halves with OD, reflecting better recovery. This register study bypasses ethical and feasibility problems og long-term studies.
This register study reflects reality/facts about Finland on national level. Treatment as usual is falsified as the most effective treatment. RCTs could give further information which of Open dialogues approaches e. g. reduction of antipsychotic medication, immediate help within 24 hours, social network perspective, dialogue etc. contributes to the good treatment results.
Scientific studies can only explain reality not disprove. Respect of reality could considerable improve treatment and health of patients. Therefore I have asked Norwegian research institutions in 2018 to do further studies on a shift of Paradigm: Can Open dialogue improve recovery rate, reduce schizophrenia per year and reduce allowance/sickness?
Later a "Call for Studies to Find out why Open Dialogue Achieves better Results" to US National Institutes of Health, UK National Institute for Health Research Norwegian Psychiatric Society (Npf) and NORMENT: Norwegian Centre for Mental Disorders Research has been made: http://wkeim.bplaced.net/files/recovery-call.html .
Both National Institute of Health Research (NIHR) and The Institute for Dialogic Practice, Northampton MA already conduct research.
Would research with focus on recovery on the basis of exploring promising treatment results of Open dialogue be the way forward to promote and improve patients health?
Walter Keim
Rindal, 6. May 2019
Reference:
Bergström et al. 2018: The family-oriented Open Dialogue approach in the treatment of first-episode psychosis nineteen-year outcomes: https://www.researchgate.net/publication/327739553_The_family-oriented_Open_Dialogue_approach_in_the_treatment_of_first-episode_psychosis_nineteen-year_outcomes
Robert Whitaker - May 21, 2017.2. Psychiatry Defends Its Antipsychotics: A Case Study of Institutional Corruption: https://www.madinamerica.com/2017/05/psychiatry-defends-its-antipsychotics-case-study-of-institutional-corruption/ shows shortcomings of Goff et al. 2017: The Long-Term Effects of Antipsychotic Medication on Clinical Course in Schizophrenia:
They never provide data from the studies showing that 60% or so of first-episode patients may recover without the use of antipsychotics.
They always dismiss the better outcomes for unmedicated patients in cited studies, arguing that it is an artifact of an unequal comparison for some reason or another (Schooler, Rappaport, Harrow, and Moilanen).
They report no data from modern longitudinal studies that tell of much better long-term outcomes for the unmedicated patients.
In their discussions of drug-induced brain shrinkage and dopamine supersensitivity, they fail to discuss information from the larger body of scientific literature essential to assessing whether these drug effects could explain the poor long-term outcomes seen in the longitudinal studies.
Robert Whitaker September 22, 2017. Thou Shall Not Criticize Our Drugs:
The letter submitted by Robin Murray and colleagues: Don’t dismiss the adverse effects of long-term antipsychotics in animal studies.
The letter submitted by Joanna Moncrieff and Stefan Priebe: Patients deserve more evidence
Answer NORMENT: “Your message for list norment@medisin.uio.no has been rejected by the moderator.”
Results of long-term use of antipsychotic drugs: